
Foreword - Alice Wiseman, Gateshead Director of Public Health
This report includes descriptions of difficulties with trauma, mental health, drug and alcohol use disorders, and deaths caused by alcohol, drugs and suicide. There are anonymised recordings and quotes of real experiences by people who have been affected. We understand that this may be difficult to hear and read.
If something you hear or read connects with you in a difficult way or brings up strong feelings, please know that you are not alone, and support is available.
Welcome to my 2024 annual report as Director of Public Health for Gateshead. Before I start, I want to highlight that the topic of this report has been very challenging to write so I understand it will be very difficult to read. However, this is something we need to talk about as it impacts many people across Gateshead, in very different ways.
In case anyone feels they need additional support; we have provided some links to support services. Please do reach out and don't suffer alone.
Lives lost too soon
The report addresses an issue of profound importance: the devastating toll of deaths caused, in Gateshead, by drugs, alcohol and suicide.
Too many lives in Gateshead are cut short because of alcohol, drugs and suicide. Sadly, we are seeing increasing harm, particularly in relation to drug related deaths. Deaths of this nature are both a consequence and cause of health inequalities. Whilst harm from alcohol, drugs and suicide can affect everyone, those in our most disadvantaged communities are hardest hit.
Hearing from people with lived experience
Numbers and data are not enough to understand this issue properly. Behind each number is a story of lives lost too soon, of loved ones left behind, and of communities grappling with pain and loss - the ripple effects are far reaching - an issue cutting across families, communities, and wider society.
My purpose in writing this report is not only to illuminate the urgent need for change while honouring the humanity which sits behind the data. Threaded through the report are the voices and experiences of people with lived experience.
It is critical that we give those affected the opportunity to share their story and to hear their voice. To understand the journeys they have experienced, and to heed their messages of hope. The need to work together with those who have lived experience to ensure that our plans and services put people and families at the heart of what they do.
Stigma
We have heard how these deaths may evoke feelings of shame, stigma, anger and guilt, adding to the pain and loss of those left behind. We need to address this stigma head on, and we need to understand how the language we use, often without realising, affects the care giver, deter help seeking behaviour and increase isolation.
The need to challenge stigma and reframe our messages around this issue, removing any blame from individuals and instead, acting on the factors that lead to these experiences and inequalities.
Influences
Harm and death by alcohol, drugs and suicide are influenced by a range of complex factors at a societal, community and individual levels including, poverty, inequality, childhood experiences, insecure work and unemployment, homelessness, social and cultural norms (including gender norms), commercial determinants such as alcohol, gambling and social media, relationship break down, domestic abuse and access to services.
Finally, the experience of death, loss and grief is, in itself, a determinant of health, for those bereaved by alcohol, drugs and suicide, the impact may be even greater. There is a need for support after bereavement, and a compassionate town approach to help recognise this, and mitigate the impacts.
Prevention
We need to focus on prevention by continuing our commitment and drive in delivering the Health and Wellbeing strategy, taking action across the eight policy objectives.
Support and recovery
We need to recognise the importance of services in reducing harm and helping people to recover, but the need to ensure we push further upstream in addressing root causes that create the circumstances which make people more vulnerable to these harms.
Conclusion
The challenges we are facing touch us all in some way, reminding us of the urgent need for compassion, understanding and action.
The report aims to set out the complex web of factors driving these tragedies, highlight the hope we have for something different and the action we need to take to get there.
While the path forward is not without challenges, its one paved with hope, hope that together we can create a future where fewer lives are lost and where prevention, support and healing are accessible to all.
To those who have been affected by this, and those who have generously and bravely shared their stories, we see you, we hear you and we stand with you. It is in your honour that we will continue this critical work.
Our lived experience (lived experience stories)
Lived Experience involvement in this report
People with lived experience have an important role in shaping programmes, interventions and services. The phrase "Nothing about us, without us" highlights the importance of engaging people with lived experience (1). Their insights help address challenges and inequalities in our communities, requiring us all to work together from service commissioners, to providers, and lived experience organisations (2).
In Gateshead, people with lived experience are at the heart of our drug and alcohol services, including roles like peer supporters and recovery ambassadors. Recognising the link between addiction and mental health, mental health peer support roles are embedded in these services, offering visible hope for recovery.
Through focus groups and interviews, we heard from those impacted by alcohol, drugs and suicide, including bereaved families and individuals who faced related challenges such as poor mental health and homelessness. Each person's experiences were unique, but there were often similarities, especially around the stigma they faced. Whilst the views shared may not reflect everyone, the focus groups and interviews aimed to hear from a diverse range of experiences and communities. Throughout this report, you will see these views and experiences shared.
These conversations brought to light personal stories of struggle and resilience. While we present data about the impact of alcohol, drugs and suicide in Gateshead, we also share these real stories to amplify the voices of those affected. Though discussions were often emotional and challenging, people valued the opportunity to share their experiences and be heard. This process highlighted the importance of considering how language shapes understanding and impacts individuals and communities.
We were told how negative, stigmatising language can create feelings of shame and isolation, while positive language made people feel cared for and understood.
Language to use when talking about this topic put forward by lived experience participants

Our Language Matters
Whether you're texting a friend, posting on social media or talking with colleagues at work, the way we communicate about alcohol, drugs and suicide can have an impact on ourselves and our communities.
Making sure you do so safely and responsibly can reduce the stigma about alcohol, drugs and suicide, including suicidal feelings and behaviours, and encourage people to ask for help.
The way we describe people with lived experience matters. As such, the language we have used throughout this report has been chosen with careful consideration of guidance from organisations including the NHS and Samaritans.
Therefore, we ask that all terminology should be replicated exactly in any communications, including media coverage, about this report.
Most importantly, we hope the language used in this report helps anyone who has struggled to find the words to talk about alcohol, drugs and suicide to feel more confident to speak out, fight stigma and empower people to seek support.
Introduction
In Gateshead, lives are being cut short by health inequalities. Those in our most disadvantaged communities face shorter lives and in poorer health. Each life lost affects not just the individual but ripples through families and communities. Tragically, many of these deaths are due to alcohol, drugs and suicide, and may bring complex feelings of stigma, shame, and guilt that deepen the pain.
The ripple effect from people that were affected, you're talking about the whole street. My immediate family, my sister, my husband, my children, my sister's children, me, auntie and uncle, my cousin, even the first responders, you know, everybody that was involved has been affected.

Between 2019 and 2021, 46,200 people in England died due to alcohol, drugs and suicide - an average of 42 lives lost every day (3). In Gateshead alone, 239 residents died during this period, about 80 people per year. The North and coastal areas experience higher rates of these deaths compared to other parts of England (3).
For adults under 50 in Gateshead, alcohol, drugs and suicide are leading causes of death (4). Researchers refer to these deaths as "Deaths of Despair", reflecting the emotional and mental distress behind them. This term originated in the United States in 2015 and highlights rising mortality linked to alcohol, drugs and suicide, particularly among middle-aged people (5). Studies suggest these deaths are tied to social and economic conditions (3), and alcohol and drugs themselves are significant risk factors for suicide (3,6), and related risks like intoxication, long-term dependence and self-harm (7,8). Understanding these risk factors can help reduce health inequalities and support people to live longer, healthier lives in Gateshead.
This report examines the scale and impact of alcohol, drug and suicide-related deaths in Gateshead. It highlights the importance of language in discussing these issues. While the term "Deaths of Despair" resonated with some of those with lived experience that we consulted, it evoked difficult and mixed emotions. However, "despair" seemed to reflect the experiences of our communities; therefore, we have chosen the term "Ripples of Despair" for this report.
Sadly, these deaths are just the tip of the iceberg. Alcohol contributes to over 60 health conditions (9), with Gateshead recording 5,326 alcohol-related hospital admissions in 2022-2023 - one of the highest rates nationally (10). During the same period, 1,260 people accessed specialist drug treatment services (11), and estimates suggest 1,716 Gateshead residents were affected by opiate and crack use (12). Gateshead also has higher-than-average rates of self-harm, with 150 hospital admissions for self-harm among 10-24 year olds in 2022-2023 (13,14). Health inequalities worsen these challenges, with some groups and communities in Gateshead more affected than others.
Behind these statistics are real people, lives, families and communities. This report seeks to share their voices, illustrate the scale of this issue in Gateshead, and explore both the challenges we face and the opportunities we have to make a difference.
The local picture; deaths by alcohol, drugs and suicide in Gateshead

The statistics surrounding alcohol, drugs and suicide paint a stark picture of loss in Gateshead.
Between 2003 and 2023, 307 lives were lost to suicide in Gateshead (15). To put the number of suicides over the last two decades into perspective, the figure is nearly three times the number of road traffic deaths in the same period (16).
In addition, 321 people in Gateshead died from drug-related causes (17), and 667 more from alcohol-specific conditions over the same time period (18).
It is important to note that alcohol-specific deaths only account for issues like liver disease, leaving out broader alcohol-related harm such as heart disease or cancers. The true toll of alcohol is likely far higher (19).

In more recent years, the COVID-19 pandemic had a significant impact on alcohol-specific deaths. Nationally, the sharp rise in alcohol-specific deaths during the pandemic was linked to increased alcohol consumption, especially among those already drinking heavily (20). Shifts in drinking habits, like more regular drinking at home, have deeply rooted alcohol in daily life, increasing its harm (21).
Sadly, Gateshead has experienced rising numbers of deaths from alcohol, drugs and suicide. For alcohol-related deaths alone, there were 283 deaths from 2020 to 2022, equating to 52.8 deaths per 100,000 people (10). In comparison, the North East's rate was 49.7 and England's was 39.7 per 100,000 people (10).
Unfortunately, since 2012, Gateshead's suicide rate has risen, aligning with national trends. From 2021 to 2023, 50 people died by suicide in Gateshead, a rate of 9.5 per 100,000 persons over 10 years old, similar to the England rate of 10.7 and North East's rate of 13.8 (22).
Potential years of life lost
These deaths disproportionately affect younger and middle-aged people, cutting lives tragically short. The years of life lost (YLL) metric measures the years a person could have expected to live, had they not died prematurely, highlighting the societal and economic impact of preventable deaths linked to alcohol, drugs and suicide.
Between 2020 and 2022, suicide in Gateshead resulted in 569 years of life lost, equating to 39.2 years for every 10,000 people, significantly higher than the England average of 34.1 (23,24).
Life lost to alcohol is even higher. In 2022, Gateshead had a high rate of potential years of life lost to alcohol, with 2,078 years lost per 100,000 males and 489 years lost per 100,000 females (9). For potential working life lost due to alcohol (before the age of 65), Gateshead males had the highest rate in England at 1,033 potential working years lost per 100,000 males (9).
Data on years of life lost due to drug use in Gateshead is limited. However, given the high number of drug-related deaths and the similar age range of those affected as seen with suicide, the impact on years of life lost is likely comparable, if not greater.
Alcohol and drugs are leading risk factors for death among people under 50 in Gateshead, with these risks escalating over time. In 2021, drug use contributed to 19.7 deaths per 100,000 - a 339% increase since 1990 (4). Meanwhile, alcohol-related deaths rose to 13.2 per 100,000, a 57% increase since 1990 (4).
Gateshead is falling behind the rest of England in these areas. The numbers show a growing need for action.
Deaths in drug and alcohol treatment
When people are engaged in treatment, their risk of drug or alcohol related death is reduced.
However, being in treatment does not mitigate risk entirely, as there can be other factors that can contribute continuing drug and/or alcohol use, along with other health vulnerabilities.
People may still die prematurely, even when accessing treatment and support. Between 2019 and 2022, and 2021 and 2022, there were 58 deaths among those in drug treatment and 15 among those in alcohol treatment (25). These figures were higher than in the previous period of 2018 to 2019. While not all deaths in treatment are directly attributable to substance use, it is often a contributing factor to health inequalities and premature death.
Deaths while accessing mental health services
Almost a third of those who died by suicide after contact with drug and alcohol services had also engaged with mental health services in the previous year (26). High rates of self-harm were also common (26). highlighting the need for stronger collaboration between drug and alcohol services and mental health services to mitigate ongoing risk, even once treatment is completed.
Things that made my drinking worse were bad situations. I had no coping mechanism for them.
The vulnerabilities of those accessing mental health services also mirror these concerns. Most patients who die by suicide share overlapping vulnerabilities, such as a history of self-harm (63%), more than one mental health diagnosis (54%), living alone (48%), and substance using involving alcohol (47%) or drugs (38%) (27).
In 2021, the UK saw 74 suicides by people who were mental health in-patients, accounting for 4% of all patient suicides. 12% of all patient suicides were by people who had been discharged from mental health in-patient care within the previous three months, the highest risk being the first 1-2 weeks after discharge with the highest number of deaths overall occurring on day three post-discharge (27).
These figures underline the importance of tailored suicide prevention efforts within mental health care. The Suicide Prevention Strategy for England: 2023-2028 outlines key actions, such as follow-up support within 72 hours of discharge and co-designed solutions with those with lived experience, to reduce preventable deaths (28).
Every life lost in Gateshead presents a chance to do better, together. Deaths resulting from alcohol, drugs and suicide are critically high in our region and often interlinked, reflecting the multiple challenges and disadvantages faced by many in our communities.
These overlapping vulnerabilities require a joined-up preventative approach which not only tackles the root causes of harm but strengthens support for those at risk. Change is both urgent and possible - we cannot afford to let these trends continue to rise.
The importance of prevention
In Gateshead, a confidential Drug-Related Death (DRD) review is conducted after every suspected drug-related death to identify patterns and opportunities for intervention. This collaborative process involves both statutory and non-statutory partners, all working to reduce the devastating impact of drug-related deaths on families and communities. With new national guidance, like the Preventing Drug and Alcohol Deaths: Partnership Review Process (28), there is an opportunity to improve the DRD review process in Gateshead, allowing for shared learning to better prevent these tragedies.
While reviews of drug-related deaths provide valuable lessons, the rising numbers in our region show that earlier intervention is essential.
Alcohol and drug dependency rarely occur in isolation - they are both causes and consequences of multiple disadvantages and inequalities, leading to interlinked vulnerabilities. Addressing these challenges requires a focus not just on treatment but on prevention, tackling the root causes of substance use and supporting people long before they reach crisis point.
Case study - Speak Their Name memorial quilt

The 'Speak Their Name' memorial quilt was created by those in the North East bereaved by suicide, with over 200 people attending workshops across the region to craft 120 individual fabric squares.
Working as both a suicide prevention initiative as well as a tribute to lost loved ones, the quilt toured public spaces with the intention of promoting hope and healing.
The project has been led by Tracey Beadle from the charity Quinn's Retreat and Suzanne Howes. Both have lost children to suicide and are determined to make a difference by bringing hope to those feeling lost, in their children's names.
The building blocks of health and wellbeing

Our health and wellbeing is shaped by many factors, starting even before we are born. These factors include where we live, the quality of our housing, our friendships and family, experiences at school, access to good jobs, and whether we have enough money to meet our needs. Together, these are the building blocks of health.
When building blocks are missing or broken, they can have a damaging effect on our health. For example, a baby born in one of Gateshead's most deprived areas is expected to live nearly 12 years less than a baby born in one of the least deprived areas.

Differences in these building blocks lead to health inequalities, which are unfair differences in health outcomes between groups of people. Deaths from alcohol, drugs and suicide are marked by these inequalities, with the highest rates of harm and death concentrated in the most disadvantaged communities.
Understanding risk factors for alcohol, drugs and suicide
A large study looking across all local authorities in England identified the following risk factors linked with deaths by alcohol, drugs, and suicide (3):

*(routine task jobs which do not require any educational qualifications)
These risk factors are shaped by the circumstances in which people live - the building blocks of health. The model below draws on several studies to help illustrate how risk factors are influenced by a range of social, political, commercial and economic factors (29-32).

Social and political factors
The conditions in which we live, learn, work and age, are shaped by social, economic and political factors (33). Changes to these factors can significantly impact our health. For instance, suicide rates often rise during times of economic recession, as financial insecurity and job losses increase stress and feelings of hopelessness (30,34). Policies such as austerity measures, interest rate hikes and cuts to public services place additional pressure on those already facing socioeconomic disadvantage. Families struggling to make ends meet may face the risk of homelessness, food insecurity, and other challenges that contribute to mental distress. These stressful life events not only worsen mental health but also increase the risk of suicide (30,34).
Media landscape
While the online world can provide valuable resources for connection and support, it also poses significant risks. Social media can expose vulnerable individuals to harmful content, including material that glorifies self-harm or provides information about suicide methods (35,36). A recent study found that 83% of people had encountered self-harm or suicide content on social media without actively searching for it, with 75% first seeing this content at age 14 or younger (36).
Young people are particularly at risk, as they may be influenced by celebrities and influencers who normalise risky behaviours like substance use. This can harm mental health and increase the likelihood of suicidal thoughts or behaviours (37).
There has been emerging evidence of the link between the online environment and suicide across all age groups, with suicide-related internet use featuring in 8% of suicides by people accessing mental health services between 2011 and 2022 in the UK (38). This includes accessing information on suicide method, visiting pro-suicide websites and communicating suicidal intent online. These people were most often aged 25-44 years (42%) and aged 45-64 (33%) whilst 18% were under 25 (38).
There is growing awareness of the role the online world plays in self-harm and suicide (39). The Online Safety Act 2023 aims to create safer online spaces by making it illegal to promote or encourage serious self-harm (40). Additionally, organisations like Samaritans have created guidelines to promote responsible reporting of suicide in the media, aiming to reduce further harm (41,42).
Commercial factors
Our last report showed that health is shaped by commercial influences, such as the availability, price and marketing of products. Industries like alcohol and gambling often glamorise their products, normalising harmful behaviours and increasing risks, including addiction and suicide (36). These industries also work to undermine awareness of the harm they cause, often funding campaigns with mixed messages, like promoting "responsible use" while embedding their products as central to our social lives (29,30,43).
This influence deepens health inequalities. Gambling venues, for example, are disproportionately located in areas of deprivation, targeting vulnerable communities (44). Gambling-related harms include financial hardship, relationship breakdowns, mental health issues and a higher risk of substance use (45).
There is growing evidence of the relationship between gambling, self-harm, and suicide (45,46), as well as how gambling and substance use exacerbate each other (44,45,47-50).
The workplace is another commercial factor influencing health. Good jobs can provide financial security, build confidence and strengthen social ties, protecting mental health (33). In contrast, poor working conditions or insecure employment can harm wellbeing, increasing stress and anxiety (33).
Community factors
Where we live has a significant impact on our health. Disadvantaged urban environments with high levels of noise, crime, rubbish and limited green spaces can increase psychological distress and depression, both risk factors for drug-related deaths and suicide (51,52). There are links with suicidal behaviours being increased when experiencing poverty and deprivation at an individual level, along with living in a more deprived community (53).
Deaths to alcohol, drugs and suicide are not equally distributed across England. Like many health outcomes, there is a marked North-South divide as well as a Coastal-Inland divide (3). Between 2019 and 2021, the rate of deaths by alcohol, drugs, and suicide was highest in the Northeast (54.7 deaths per 100,000 people). The rate in Gateshead was 48.7 deaths per 100,000 people, significantly above the England rate of 33.5 per 100,000 population. The geographical inequalities are visualised in the map below.
Map of age-standardised mortality rate for deaths of despair across local authorities in England (2019-2021)(3).

The relationship between deaths by alcohol, drugs and suicide and factors such as living alone, living in an urban environment, being economically inactive, and unemployment are amplified in the North of England compared to other parts of England (3).
When looking at deaths due to alcohol, drugs and suicide in isolation, the geographical picture is very similar. The North East has the second highest rate of deaths by suicide of any region in England and Wales in 2023 (14.5 deaths per 100,000 people) (54,55).
The North East is the region with the highest rate of deaths due to drug use (10.9 deaths per 100,000 in 2023); this has been the case for the past eleven years (56).The alcohol-specific death rate is also highest in the North East (20.4 deaths per 100,000 in 2021), as it has been for the seven preceding years as well (57).
Social cohesion and fragmentation
Areas with high social deprivation and low community cohesion, such as places where people frequently move in and out, or many single-person households, are more likely to see higher rates of drug-related deaths and suicide (52). By contrast, strong social ties and support networks, often referred to as social capital, act as protective factors, reducing the risk of harm (34).
VCS case study - Edberts House
Established in 2009, Edberts House is an organisation working with over 4000 people across Gateshead.
Their four community houses offer individual support and group activities, including men's groups, refugee support group, training courses and children clubs. These have encouraged residents to have autonomy over decisions affecting their lives, as well as strong partnerships across the wider community, supporting residents' mental health in particular, and improving social connections, forming relationships with groups of people residents would not usually interact with. It has had strong positive outcomes since its inception, with those involved in one of their houses reporting life satisfaction on a par with the English national average, whilst outperforming scores for levels of trust, sense of belonging and levels of anxiety (58).
Their Community Linking Project offers social prescriptions to patients of 25 GP surgeries in Primary Care, addressing the wider determinants of health, such as housing, finances and loneliness. Their Health Equity project tackles health inequalities, including their children, young people and families team, who build trusting relationships, asking 'what matters to you?' and work with people to achieve their dreams. Knitting people together in peer support groups is a vital part of this approach - building connection and healthy interdependence. Innovative social prescribing work in secondary care is now being piloted, including their Palliative Care Link Worker, and Midwifery Social Prescribers. Evidence collected through the project has been analysed by Northumbria University, and has demonstrated that the interventions, advice and/or support provided by Edbert's House yielded a statistically significant improvement in emotional well-being.
Individual factors
The challenges individuals face are deeply shaped by their circumstances. Poverty, discrimination and abuse are just some of the structural issues that increase vulnerability. Life events like relationship breakdowns or homelessness can add to the risk of harm from alcohol, drugs and suicide. For those experiencing multiple disadvantages, these risks often overlap.
Children and young people: adversity, trauma and building resilience
The foundations for lifelong health and wellbeing are laid in early childhood. Positive experiences during this time are linked to better social and emotional development, stronger educational outcomes, and improved long-term health, including longer life expectancy (58,59). Conversely, adverse childhood experiences (ACEs), such as trauma, abuse, neglect or challenging environments, can lead to poorer outcomes like mental health challenges, unemployment, substance use, and homelessness (60,61).
The impact of adversity
While ACEs do not guarantee negative outcomes, they significantly increase the risk, particularly for children who face multiple adversities or live in poverty (62,63). Research shows that 85% of people in contact with criminal justice, substance use, and homelessness services experienced childhood trauma (64). Children who have been exposed to four or more ACEs as particularly vulnerable to poor health outcomes across the life course (65). However, many children overcome adversity when they have access to protective factors like stable relationships, supportive caregivers, and safe environments (60,63).
The pressures of child poverty, the cost-of-living crisis, and the lasting effects of the COVID-19 pandemic have increased these issues in the North, where child poverty rates exceed the national average (66).
For example, in Gateshead, the rate of alcohol-specific hospital admissions for under-18s is nearly double the England average, highlighting the urgency for action.
Care-experienced children and young people
Care-experienced individuals are those who have spent time in foster care or children's home, and they face significant health and social inequalities (67-69). The factors underpinning and exacerbating these inequalities are often rooted in trauma and adverse childhood experiences and linked closely with poverty, education, housing, and many other building blocks of health (70).
They are at higher risk of mental health challenges, substance use, and premature death, often from "unnatural causes" like suicide or drug-related deaths (67,68,71,72). Children in care, often due to the trauma of abuse or neglect, may experience greater levels of drug and alcohol harm compared to their peers and are over four times more likely to attempt suicide than their peers (73,74).
Building resilience
Resilience is the ability to adapt to stress and adversity, and it can protect children from long-term harm. Positive relationships with parents, caregivers, friends, teachers, and wider support networks are critical, as they provide the stability and support needed to develop coping skills and build self-esteem (64). Building resilience is not a quick fix. It requires sustained, long-term support and interventions (3). Resilience-building strategies include:
- Creating safe, trusting environments for children
- Providing opportunities to build self-esteem and a sense of control
- Strengthening family relationships and addressing household challenges
- Offering community-level support and services to address broader inequalities
Gateshead's Health and Wellbeing Strategy reflects this commitment, prioritising "giving every child the best start in life", with a focus on conception to age two as a critical period for intervention (75). The Early Help Strategy (2023-26) builds on this by expanding Family Hubs and programmes to support family stability and reduce risks before they become set in.
By addressing individual and community risk factors, Gateshead aims to create environments where all children can thrive, breaking cycles of adversity and promoting wellbeing for generations to come.
Case study - Trusting Hands Gateshead
Trusting Hands Gateshead (THG) is a multidisciplinary team of mental health practitioners, employed by the Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust (CNTW), THG works with Gateshead Children's Social Care services to deliver trauma-informed care.
The service name, 'Trusting Hands Gateshead: Strengthening connections through stories, safety, compassion and care', was developed with input from young people in Gateshead residential care homes, supported by Gateshead Young Ambassadors.
THG aims to:
- Understand and address the emotional and mental health needs of vulnerable young people
- Support families and systems around young people to promote stability and resilience
- Enable young people with complex needs to thrive
Demographics
Age
Deaths due to alcohol, drugs and suicide are most common in middle age. Between 2019 and 2021, the highest mortality rates were among 45-60-year-olds (3). While middle-aged adults have the higher number of deaths, young adults face a disproportionate risk: alcohol, drugs and suicide accounted for 41% of all deaths among 25-29-year-olds (3).
Generation X, who are those born in the 1960s and 1970s have continued to have high rates of deaths from drug poisonings and suicide for the past 30 years (76). This may be linked to opioid use and the increasing health effects of ageing (76,77), alongside experiences of risks such as financial instability, and unemployment (76). This evidences highlights the need for action to protect future generations when facing adversity.
Ethnicity
Suicide and alcohol-specific deaths are most common in White and Mixed/Multiple ethnic groups, with Indian males also experiencing elevated alcohol-related death rates (78,79)
Alcohol-specific deaths age-standardised mortality rate per 100,000 in England and Wales 2017-2019 (79)
| Ethnicity | Males | Females |
|---|---|---|
| White | 15.3 | 8.1 |
| Mixed/Multiple Ethnic Groups | 12.5 | 8.2 |
| Indian | 16 | 1.9 |
| Bangladeshi | 0 | 0 |
| Pakistani | 2.5 | 0 |
| Asain Other | 7.5 | 1.5 |
| Black African | 2.5 | 2.2 |
| Black Caribbean | 3.3 | 2.4 |
| Black Other | 6 | 2.7 |
| Other ethnic group | 4.8 | 0.9 |
The National Programme on Substance Use Mortality data from 1997 to 2023-2024, indicates that where ethnicity is known and recorded at death registration, the majority of deaths involving illicit substances are among those of white ethnicity at 96.1% (80).
However, ethnicity data is often incomplete, and 30% of drug-related death records lack this information (80). Barriers to care and targeted support for ethnic minority groups remain a significant concern.
Sex
Across all three causes, most deaths are among males. In 2022, across England and Wales, males accounted for three-quarters of suicides, two-thirds of all drug poisonings, and two-thirds of alcohol-specific deaths (28,29).

Women between the ages of 16 and 24 are almost three times as likely (26%) to experience a common mental health issue as males of the same age (9%), and women are twice as likely to be diagnosed with anxiety as men (82,83). However, women are more likely to seek support (84).
Men in the UK have reported lower levels of life satisfaction, happiness, and the feeling that what they do in life is worthwhile, than women, according to the national wellbeing survey 2016-17 (85). Men are also less likely to seek help, often using substances as coping mechanisms for poor mental health, exacerbated by gender norms that discourage vulnerability (84) (86).
LGBTQ+ community
Lesbian, gay, bisexual, trans, queer, and questioning (LGBTQ+) people face significant health inequalities throughout their lives. (87) Discrimination (both within and outside of healthcare), unmet needs, barriers to accessing appropriate support and negative experiences when accessing support all contribute to worse health outcomes.
It is difficult to assess rates of deaths due to alcohol, drugs, and suicide for those who identify as LGBTQ+ in the UK as sexual orientation and gender identity are not recorded on death certificates. (88) However, research in this area suggests the LGBTQ+ population experience a higher risk of mental ill health, self-harm, and suicidal behaviour (88), in addition to higher levels of hazardous drinking and illicit drug use (89-91). Inequalities in access to healthcare exist for the LGBTQ+ population and these barriers to care impact people accessing the support they need (88,89).
Neurodivergence
Neurodiversity is a term used to describe the natural variations in the ways all our brains work (92-94). Neurodivergence includes Autism, Attention Deficit Hyperactivity Disorder (ADHD), Tourette's Syndrome, Dyslexia, among other conditions. Research indicates that autistic people are more at risk of suicidal ideation and attempted suicide than the general population, and the number of autistic people dying by suicide is approximately 2-8 times higher than those who are not autistic (95).
Potential underlying factors, specific to autism, which may increase suicide risk include masking or hiding autistic traits to fit in, which is detrimental to mental health, repetitive thoughts which can lead to rumination and feeling trapped; and lack of appropriate support (95). Autistic people have been identified as a priority group in the national suicide prevention strategy (96).
ADHD is also linked to an increased risk of suicidal ideation and substance use due to co-occurring mental health challenges like anxiety and depression (97-105).
Pregnancy
Perinatal mental health issues impact over 1 in 4 pregnant women and new mothers (106) and suicide is the leading cause of death during the period from 6 weeks to 1 year postpartum, with an increased risk for women facing multiple adversities (107,108).
For women experiencing drug and or alcohol issues, there is an intense stigma around pregnancy, birth and postnatal. It can be difficult to access the support they need to manage their mental health whilst caring for themselves and their children. Some mothers face the additional trauma of their children being removed (107). Pregnant or postnatal women who are experiencing adversity and disadvantage often experience feeling judged, misunderstood, shame and guilt. This can subsequently exacerbate their struggles with substances and contribute to further deterioration in their mental health (107).
Health status
Conditions such as chronic pain and respiratory illnesses like chronic obstructive pulmonary disease (COPD) are common among those with substance use issues (109,110). Chronic pain doubles suicide risk and can lead to substance use as a coping mechanism, further complicating care (109,111). For example, approximately 50% of alcohol and drug use disorder patients are affected by chronic pain (109).
Mental health and self-harm
Around 1 in 4 suicides in England are people who are known to mental health services(96).Mental health conditions such as borderline personality disorder, anorexia nervosa, depression, bipolar disorder, and schizophrenia increase suicide risk (112). Dual diagnosis is where substance use disorder and mental illness co-occur, this can present additional barriers to care, as services often focus on one issue rather than addressing both simultaneously (113,114).
Self-harm is "an intentional act of self-poisoning or self-injury, irrespective of the motivation or apparent purpose of the act and is an expression of emotional distress" (115) and is a major risk factor for suicide. In Gateshead, emergency hospital admissions for self-harm are significantly higher than the national average (14), particularly among young people aged 10-14 where it is double the rate in England (116), indicating a critical need for mental health support locally.
Socio-economic position
Poverty
Living in poverty impacts people, and their health, throughout their lives (58). It goes beyond a lack of money—it's the constant stress, scarcity of resources, and loss of control and dignity that take a toll on mental and physical health. Living with debt is particularly damaging, linked to adverse outcomes, including deaths due to alcohol, drugs, and suicide (58). This constant strain, known as economic adversity, forces people to focus on immediate survival, often leaving little capacity to plan for the future.
The graphs below show the link between deprivation and death by alcohol, drugs and suicide. The most deprived 10% of areas have markedly higher rates of deaths from alcohol, drugs, or suicide than the least deprived 10% of areas.
Alcohol-specific mortality in England in 2021(directly standardised rate per 100,000, County & UA deprivation deciles IMD 2019, 4/21 geography).
(117)
Those with lower socio-economic status suffer greater harm from alcohol, even though they tend to drink similar or lower amounts compared to wealthier groups - a phenomenon known as the "alcohol harm paradox". (118,119)
This highlights how other factors, such as access to healthcare and nutrition, may amplify the risks for populations experiencing deprivation.
Deaths from drug use in England in 2020-2022(Directly standardised rate - per 100,000, County & UA deprivation deciles, IMD 19, 4/23 geography)

(120)
For deaths by suicide, the County & UA deprivation deciles do not demonstrate the same trends, potentially due to lower numbers of deaths across large geographic areas masking inequalities. Suicide also occurs at higher levels in some rural areas, which are generally less deprived (52,121). However, there is a clear difference of rates by level of deprivation when looking at data for smaller local areas (LSOAs).
Suicide rate in England 2019-2021(persons 10+ years, directly standardised rate per 100,000, LSOA 11 deprivation deciles IMD 2019)

(22)
Insecure work, low wages, cost of living, inflation, insufficient benefit provision all contribute to an economic landscape where poverty and deprivation are unavoidable for many (58). Unfortunately, the reality is not as simple as finding a job and earning enough money to move out of poverty. We know that more people are working and remain in poverty (58,122).
Employment status
Unemployment is strongly linked to poor mental health and is a risk factor for harmful drinking, drug use, suicide, and homelessness (123-125). During times of economic recession, unemployment often leads to psychological distress, which increases substance use as a coping mechanism. During these times, providing psychological support for those who have lost their job and are vulnerable to drug use is essential (126).

The Dame Carol Black review highlighted employment is an essential part of recovery from substance use, for both financial stability and to offer something meaningful to do (127).
According to the World Health Organization, decent work can improve mental health, but also provides a sense of purpose, confidence, and routine. It builds social connections and supports recovery for those with mental health or substance use issues (128).
However, people with drug issues face significant barriers to employment, including stigma, receiving treatment whilst working, mental and physical health challenges, and lack of skills or training. Addressing these obstacles requires both individual support and broader societal changes (129). Rates of employment for people with severe mental illness are particularly lower than for any other group of health conditions, underscoring the need for tailored interventions (130).
Case study - Individual Placement Support (IPS)
Gateshead & South Tyneside's Individual Placement Support (IPS) initiative connects job seekers in recovery from addiction with meaningful employment opportunities. Embedded within local drug and alcohol services, IPS has helped over 100 individuals secure sustainable jobs.
Across the two local authorities, the team believes that everyone in our communities deserves a fair chance, so works hard to help people in recovery to find meaningful and sustained work. Employers are also a key part of supporting the initiative, and work with Gateshead & South Tyneside IPS to offer new roles and opportunities throughout the year.
Contextual factors
Stressful life events such as relationship breakdowns, chronic illness, or bereavement can increase susceptibility to substance use disorder and suicide. (131,132) Childhood maltreatment is also a significant risk factor for early substance use and long-term alcohol problems (131). While these factors do not guarantee harm, understanding them helps target resources and support where they are most needed.
Exposure to conflict, violence and war: asylum seekers and refugees
Inequalities experienced by refugee and asylum-seeking populations throughout their lives may contribute to factors increasing risk of harm by alcohol, drugs and suicide. While refugee and asylum-seeking communities are diverse groups, people that have been displaced are likely to have common experiences related to being on the move.
Factors during migration journeys may include issues such as poor living conditions and fears that come with being trafficked. They may feel a sense of shame, or guilt, at having to have fled their country of origin - perhaps leaving loved ones and their homeland behind. Their living standards may be drastically different from their home country, lacking basic services and often experiencing violence and detention (133).
Stigma may be felt by those with a refugee and migration background upon their arrival into their host country. This may be surrounding barriers to accessing healthcare and other services, poor living conditions, separation from support networks and family, uncertainty surrounding work permits and legal status, and in some cases, immigration detention (133). There are also challenges around adapting to change, potential unemployment, racism and exclusion, social isolation and possible deportation (133).
Poor mental health is common and may include symptoms of anxiety and depression, PTSD, suicidal ideation and/or attempts, along with substance use disorders (134). Substance use is often initiated or increased after experiencing trauma, to self-medicate and avoid difficult emotions (134). Women and unaccompanied minors are particularly vulnerable, facing risks such as exploitation and harassment, correlating with substance use (134).
Exposure to conflict, violence and war: veterans
Veterans experience higher rates of depression, Post Traumatic Stress Disorder (PTSD), and alcohol misuse compared to civilians (135,136). PTSD in particular can co-occur with problematic alcohol use (135,136).
Services like the Armed Forces Outreach Service and Walking with the Wounded report that alcohol misuse is a factor in up to 60% of referrals (137).
While suicide rates among veterans are generally lower than the general population, young early service leavers are at higher risk (137,138).
Domestic abuse
Domestic abuse has severe physical and mental health consequences for victims and survivors. Those experiencing domestic abuse are more likely to have substance use needs and experience homelessness (139). Rates of domestic abuse in the North East are higher than England, and drug-related deaths, suicide, and domestic homicides are more common in women experiencing abuse (139).
In 2021, women in the North East of England were 1.7 times more likely to die early because of suicide, addiction, or murder by a partner or family member than in the rest of England and Wales (140).
Rates of domestic abuse related incidents and crimes have been increasing, and Gateshead has higher levels than England, with 38 incidents per 1000 people in 2022/2023 (141). Among victims and survivors in Gateshead, data shows also increasing additional needs, with mental health needs most common (139).
Tragically, suicide is increasingly recognised as a consequence of domestic abuse, with 93 of the 242 domestic abuse-related deaths in England and Wales in 2022/23 being suicides (142).
There is therefore a strong association between substance use and domestic abuse - as a risk factor for perpetration and victimisation of domestic abuse. Perpetrators of domestic homicide have been found to have high rates of alcohol and/or drug use (143-146).
Homelessness
In 2022-2023, over 1,600 households in Gateshead faced homelessness(147).Homelessness severely impacts mental and physical health, with many people experiencing substance use, mental health challenges, and trauma (148,149). Children in these households are also affected, with impacts on their education, mental health, and family stability (123).
The health inequalities and poor health outcomes faced by those experiencing homelessness are stark. For those who are sleeping rough, there are significant needs related to mental health, drugs and alcohol (148,149).

The root causes of homelessness, including poverty, lack of affordable housing, and unemployment, are intertwined with the risk factors for alcohol, drugs, and suicide (149). Addressing these systemic issues is critical to reducing harm and promoting recovery.
Experience of the criminal justice system
People in contact with the criminal justice system face significantly higher risks of suicide and drug-related deaths. Offenders in the community are approximately six times more at risk of suicide than the general population, and the risk of drug-related death amongst this population is 16 times higher (150). Female offenders are at even greater risk, with rates of suicide and drug-related deaths 11 and 33 times higher respectively than the general population.
Barriers to accessing appropriate support further exacerbate these inequalities. Addressing health disparities in this population can improve overall wellbeing and reduce reoffending rates (151).
System and service factors
Services play an important role in supporting those at risk of harm from alcohol, drugs and suicide. Recover-focused interventions that prioritise holistic joined-up care can help individuals rebuild protective factors like stable relationships, employment and housing. These services and interventions include:
Talking therapies
Talking therapies are psychological treatments for mental and emotional problems like stress, anxiety and depression. There are several different types of talking therapy, such as cognitive behavioural therapy (CBT).
Gateshead Talking Therapies offers free and confidential NHS support for those aged 16 and over who are registered with a GP in Gateshead, providing treatment to help individuals cope and recover.
Crisis support
Gateshead have four Crisis Beds for adults in mental health crises, offering short-term support for up to four weeks as an alternative to hospital admission. Staffed 24/7, these beds address urgent needs while helping to prevent acute mental health admissions.
In 2025, Gateshead will launch a Safe Haven, operating daily from 3-11pm. This service will offer rapid, non-clinical support to individuals experiencing crises, reducing distress, providing a listening ear, and offering practical guidance.
Alcohol IBA
Alcohol Identification and Brief Advice (IBA) offers simple, effective advice to individuals drinking at risky levels, helping them reduce harm (152).
While commissioned within GP and pharmacy services in Gateshead, IBA is also delivered in settings like homeless services, ensuring those not registered with a GP can access support and referrals to specialist services.
Naloxone
Naloxone is a life-saving emergency antidote to opioid overdose, temporarily reversing its effects (153). It may reduce the number of opioid related deaths, which make up the largest proportion of drug related deaths (154).
In Gateshead, Naloxone is distributed through commissioned drug and alcohol services, participating pharmacies and as part of discharge plans for at-risk patients at the QE hospital.
Employment support / IPS
Individual Placement Support (IPS) supports people with severe mental health conditions or substance use issues by helping them find and retain meaningful employment (130). Embedded within Gateshead's drug, alcohol and mental health services, IPS connects individuals with roles that match their strengths and ambitions, contribution to recovery and social inclusion.
Specialist alcohol and drug treatment services
Gateshead offers specialist treatment and recovery services for both adults (Gateshead Recovery Partnership) and young people (Positive Futures).
These services improve public health, reduce harm and generate system-wide savings by preventing costly health, social care, and crime-related issues (155).
Specialist Alcohol and Drug Liaison Nurse
Gateshead's Specialist Alcohol and Drug Liaison Nurse works within the Psychiatric Liaison Team at the QE Hospital, providing assessments, interventions and continuity of care.
By connecting hospitalised patients with community services, the nurse ensures smooth transitions and ongoing support for recovery.
Crisis team
The Newcastle and Gateshead Crisis Team offers 24/7 mental health support for young people and adults in crisis. Comprising nurses, social workers, psychiatrists, and pharmacists, the team provides assessments and home-based treatment as an alternative to hospital admission.
Alcohol Care Team
The QE Hospital's Alcohol Care Team delivers specialist interventions, including medically assisted withdrawal and discharge planning. They work closely with community alcohol services to ensure patients receive ongoing care and support after leaving the hospital.
Stigma, shame and discrimination
Part of what got me into the hole was this stigma attached with what happened to me, the stigma then attached with my mental health as a result of what happened.
Stigma, shame and discrimination deeply affect people harmed by alcohol, drugs and suicide. They shape how individuals experience these struggles during their lives and how families, friends and communities grieve after a death. Unlike other illnesses, like cancer, addiction and mental health conditions are often misunderstood, with society sometimes viewing them as issues of personal choice or control. This unfair perception creates barriers to seeking help and reinforces feelings of shame.
A recent report (156) commissioned as part of the NHS Stigma Kills campaign identified stigma as:
- Discrimination - the behaviour that resulted from the prejudice from others
- Experienced stigma - the experience of being stigmatised by other people
- Social or public stigma - the negative attitudes and prejudice held by society
- Anticipated stigma - the feelings people had when they expected to be on the receiving end of bias from other people
- Self-stigma - the internalisation of stigma felt by individuals resulting from social stigma
- Perceived stigma - the perception of how a particular stigmatised group is treated by others
Stigma is also embedded in the language, narratives and media that surround us. Labels and negative descriptors dehumanise people and shape how society views them and how they view themselves (157). For example, describing addiction as a "lifestyle choice" or mental illness as an "excuse" creates damaging stereotypes that blame individuals for the struggles they face and ignore the systemic disadvantages and traumas that contribute to these conditions.
With 'commit suicide', we talk about people committing a crime, but something about committing suicide, to me, suggests that it is in the same ballpark. It sounds like a deliberate act.
Outdated language, like "commit suicide", reflects stigma rooted in the past where suicide was a crime in England and Wales until 1961. Although attitudes have shifted, stigma around suicide and mental health remains. Research shows that 1 in 5 people will have suicidal thoughts during their lifetime and 1 in 15 will attempt suicide (82), yet most won't disclose their feelings due to fear and worry about how others will respond (158).
My cousin took her own life as a result of heroin. Her family refused to use the words 'committed suicide'; instead, they would say she 'took her own life'.
Language matters. The words we use to describe addiction, mental health or suicide can either reduce stigma or deepen it. These judgements extend to healthcare settings, where stigmatising views can influence the care people receive (159). Stigma shaped by society may be internalised. People start seeing themselves through the lens of the prejudice they face, lowering their self-esteem (160) and pushing them further into addiction and/or despair (161).
The impact of stigma and shame
Stigma has real, harmful consequences. It stops people from seeking help, isolates them from support networks, and creates barriers to treatment. (162,163) For example, men are often discouraged from expressing emotions due to traditional ideals of masculinity, making them less likely to seek help for mental health or addiction (164,165) .
For women, stigma is often tied to societal expectations about their roles. A recent study found that women in recovery from alcohol dependence described shame as stemming from failing to meet stereotypes of being a "good mother" or "ideal woman". These expectations contributed to their use of alcohol as a way to cope (166).
Mental health is also stigmatised in many parts of the world, with different cultural concepts of mental health and internalised stigma reducing people's chances of seeking adequate healthcare even when available (167). In some communities, mental ill health is not spoken about. Refugees and asylum seekers in particular can face stigma, with many fearing seeking help due to cultural taboos, mistrust of healthcare systems, fear of authority, as well as a potential lack of familiarity with treatment for these conditions (165,168,169).
Reducing stigma
Reducing stigma starts with changing how we talk about these issues. Using compassionate, non judgemental language in all aspects of our life can make it easier for people to seek help and encourage society to see addiction and mental health struggles as health conditions, not burdens to face alone.
Case study: Recovery Connections Coffee Bike

It's a simple, powerful way to make recovery visible, share support options and challenge misconceptions and stigma around addiction.
At an event held at the Quayside last summer, the coffee bike sparked 220 conversations. By chatting with people who have lived experience, many attendees changed their views about addiction and learned that recovery is possible. The bike's success demonstrates how small acts of connection can reduce stigma, spread awareness and inspire hope.
The ripple effects felt by families, communities, and society
Families
When someone dies by suicide, drugs or alcohol, the impact on their family is profound. Beyond the devastating loss, families often face stigma, shame and isolation, making their grief even harder to bear. They may feel judged by others or experience self-blame, guilt and confusion.
This stigma often leads to reluctance in talking about the loss, and some families may even conceal the cause of death (170). This silence can intensify feelings of isolation and grief, highlighting the importance of access to support services and groups (171). Grieving these types of deaths is often described as 'traumatic grief' - a prolonged and intense form of loss marked by emotions such as guilt, anger and unanswered questions (172,173).
Studies have shown that people bereaved by suicide are twice as likely to be diagnosed with depression or anxiety themselves and are at greater risk of post-traumatic stress disorder, suicidal thoughts and prolonged grief (174-176). It is widely reported that bereavement from suicide can make a person more vulnerable to suicide themselves, but it can also have a protective effect in that experiencing the loss and pain of suicide makes them feel that suicide is not something they could ever do (177-179).
For all deaths due to drugs, alcohol or suicide, the whole family is impacted, and a continuing cycle of trauma is possible if the needs of people grieving go unmet. The impact can continue to be felt in the generations that follow.
Children in families affected by addiction or bereavement face additional risks. They are more likely to experience mental health issues like anxiety and depression, struggle in school, or develop their own substance problems. Addressing these challenges through postvention support is critical to breaking cycles of trauma and reducing long-term harm (180-182).
Communities
The ripple effects of suicide, drug and alcohol-related deaths extend far beyond immediate family and friends, often impacting entire communities. these deaths are far more reaching than originally thought, extending beyond family, friends, and contacts to include people with a perceived closeness or someone who identifies with them (176).
It had been reported for decades that six people are affected by one suicide, based on the average size of immediate family (183). More recent research takes into account those wider ripples felt through the community and estimates up to as many as 135 people are affected, including acquaintances, colleagues, and even those who had limited interactions with the person, such as a familiar face in the local coffee shop or a member of the emergency services responding to the incident (184).

Using this figure, we can estimate that over the past 20 years almost 41,500 people may have been affected by suicide in Gateshead, whilst in 2023 alone around 2,160 people were potentially impacted.
People who have a close relationship with the person who died, including family members, close friends and associates, are described as 'suicide-bereaved'.
The difference between 'short-term' and 'long-term' bereaved is the prolonged and debilitating impact of the death felt by the long-term bereaved (185).
This highlights just how indiscriminate suicide is, it can affect us all in many ways.
Society
Suicide contagion
The notion that one person's suicide can influence another's suicidal behaviour is based on the Social Learning Theory; that people learn behaviours by seeing them in others. Where they identify with the person displaying the behaviours and see it as having a desirable outcome, their likelihood of carrying out the same behaviour is increased (186).
This is known as 'suicide contagion', "whereby one or more than one person's suicide influences another person to engage in suicidal behaviour or increases their risk of suicide ideation and attempts" (187).
Contagion can happen when a person is 'exposed' to a suicide either through direct exposure, such as suicide by a peer or witnessing the tragedy, or indirect exposure, such as a suicide reported in the media or identifying with the person who died. Both are reported to increase suicidal behaviour in people who are already vulnerable to suicide, especially in adolescents and young adults (132).
The impact on staff and services
Frontline workers, including those in health, social care and emergency services, often face secondary trauma from exposure to these deaths (188). Staff may experience feelings of sadness, guilt or anger, leading to burnout, compassion fatigue, or even PTSD. The practice of trauma informed care has been used to increase knowledge and understanding of trauma-based behaviours and appropriate interventions to support those using services. It is also vital that trauma related responses in the workforce are also identified and appropriate support given to the staff (188).
Gateshead Recovery Partnership offers initiatives to support staff who experience the loss of someone they've worked with, including "loss of life" forums and access to counselling through the Employee Assistance Programme. These measures provide safe spaces for reflection and support.
Emergency responders also face significant challenges, with 1 in 4 reporting thoughts of suicide linked to work-related stress or poor mental health (189). Resources like Mind's Blue Light Together platform provide crucial mental health support for those in high-stress roles (190).
The economic impact
The cost of alcohol harm in Gateshead 2021/2022, can be broken down across four areas, economy, social, health and crime, with an overall cost of £106.3 million (191).
If we consider the cost of harm relating to alcohol from a healthcare and NHS perspective, alcohol related hospital admissions, outpatient visits, alcohol related A&E visits, alcohol related ambulance call outs, alcohol-related healthcare appointments and other alcohol related healthcare costs total £21.2 million (191).
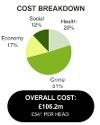

Gateshead and the North East have high rates of alcohol mortality, which results in significant levels of working life lost. In addition, the ripple effect of alcohol harms more broadly, impacts the wider economy of Gateshead, at a cost of £17.6 million related to lost productivity at work, absence from work, and unemployment (191).

For drugs, Dame Carol Black's independent review exposed the scale of the national challenge. The financial cost from the harms of drug use to society is estimated to be £19.3 billion per year, 86% of which is attributable to health and crime related costs (192). Problematic drug use is highly correlated with poverty and impacting our most deprived communities (193).
The review identified the big business of illicit drugs, estimating its worth at £9.4 billion a year. As drug related deaths have risen, the illicit drugs market has become much more violent.
For suicide, the economic impacts range from financial losses due to years of life lost in employment, impact on employment and productivity for those bereaved, costs felt by the healthcare system, emergency services, coroners and families. The average cost of a suicide in the UK in 2022 was estimated at £1.46 million by the Samaritans, with overall suicides costing £9.58 billion (194).
However, when looking at Gateshead from 2018 to 2022, the total cost is estimated at £122 million, with the average cost per suicide slightly higher than the UK rate, at £1.5 million (194). This suggests that the economic impact of suicide in Gateshead may be greater than the national average.
These figures show that suicide prevention is a crucial area for public investment due to the significant emotional and financial cost caused by suicide each year.
Talking about death - death literacy
When I said, well, actually my dad took his own life, I started to feel sorry for the people that asked that question because I could see their Persona change instantly. I could see they felt bad for asking the question or shocked.
Death is a difficult topic to discuss, yet it's an inevitable part of life. This report highlights how death impacts those affected by alcohol, drugs and suicide, and how stigma can make grieving even harder for families. "Death literacy" refers to having the knowledge, skills and understanding to support others through dying, loss and bereavement. It's an important way for communities to offer compassion and care during life's most challenging moments.
Barriers to end-of-life care for people with alcohol and drug issues
People struggling with alcohol and drug disorders are less likely to access timely end-of-life care, missing the chance for a dignified and supported death (195). This group experiences what researchers call "structural vulnerability" - a lifetime of inequalities that follow them into death. Factors like poverty, trauma and stigma amplify this vulnerability, leaving their physical, emotional and social needs unmet (195,196).
Unlike predictable disease trajectories like advanced cancer, conditions caused by drugs and alcohol often involve a more uncertain decline, making it harder for healthcare professionals to plan or initiate conversations about dying. Unfortunately, avoiding these conversations leaves individuals without the opportunity to prepare for the future or express their wishes for care. Terminal illnesses tied to drugs and alcohol also carry additional stigma. As a result, people with drug and alcohol issues often don't receive palliative care until their final days - if at all - missing out on the comfort and dignity of a well-planned death and the accompanying care (195,197).
Fear can also play a role. Research shows that some individuals delay seeking care, worried they'll be judged, denied pain relief, or required to abstain from substances before receiving help (198). For those facing multiple disadvantages, like homelessness or hunger, addressing basic needs often takes priority over health, leading to late-stage care that's often too little, too late (199).
The current system often fails these individuals. Unlike integrated cancer or palliative care services, those with illnesses caused by drugs or alcohol experience fragmented and inconsistent support. They are frequently passed between services without receiving the holistic care they need, leaving gaps in treatment and bereavement support for their families.
The importance of 'end of life' literacy
Death literacy helps people plan for, navigate and support others through dying, loss and caregiving. It includes understanding practicalities like wills and healthcare preferences, as well as emotional and social aspects of death and grief. When this literacy is lacking, people can feel unprepared and isolated, while families and friends may struggle to cope with the loss.
When I spent time with Gateshead's addictions team, I heard how often they encountered death. While staff felt unprepared to talk about it, those with lived experience were much more open. Conversations about death seemed less of a taboo in this community.
Dr Elizabeth Woods, Consultant in Palliative Medicine
Improving death literacy can empower individuals and communities to offer better support during end-of-life care. Open conversations about death, dying and grief can break taboos and dismantle stigma, creating safe spaces for closure with compassion.
Compassionate cities: a model for better end-of-life care
Compassionate cites aim to create environments where aging, dying and grieving are seen as natural parts of life, supported by the entire community. This model integrates education, awareness and practical support into everyday spaces like schools, workplaces and homes (200). Grief is often thought of only as an emotional reaction to loss. However, this narrow understanding ignores wider social consequences of loss, including anxiety, depression, loneliness, social isolation, stigma, rejection, missed work or school, and even suicides and sudden deaths which can follow on from experiences of dying.
Compassionate cities aim to acknowledge these social impacts and promote health and wellbeing through better support, information and prevention initiatives which might mitigate these challenges.
Plymouth and Birmingham, the first compassionate cities in England, have taken steps to improve end-of-life care for marginalised groups, including those with drug and alcohol addictions. Initiatives like training "end-of-life ambassadors" and hosting workshops for street pastors and addiction nurses have enabled these communities to offer better care and understanding. By normalising conversations about death, compassionate cities help to dismantle the stigma surrounding dying, loss and addiction-related deaths. These efforts not only improve care for individuals but also build stronger, more empathetic communities.
Creating a compassionate gateshead
Gateshead has the opportunity to embrace the compassionate cities approach (201), ensuring that everyone (regardless of their circumstances) has access to dignified end-of-life care. For people with illnesses related to drugs and alcohol, early conversations about planning for the worst while hoping for the best could make a significant difference. By improving death literacy and addressing the inequalities that shape end-of-life experiences through our services, charities and communities, Gateshead can become a place where every resident can live - and die - with dignity, compassion and support.
Support following bereavement (post-vention)
Postvention refers to the support offered to individuals and communities after a death by suicide. Suicide has far-reaching ripple effects, often leaving those affected struggling with grief, mental health challenges and an increased risk of suicide themselves (202).
Yet many people in our communities do not seek the support they need, with one UK study finding that 25% of people bereaved by suicide received no support at all. Those who did often faced delays or lacked informal support compared to people grieving natural deaths (203).
Lack of support is a concern, as early intervention and effective support for those bereaved by suicide can act as important means of suicide prevention in a group who are at increased risk of poor mental health, suicidal thoughts and attempts, and dying by suicide. People bereaved may need the opportunity to access support services on more than one occasion at different stages of grief (204).
There is not a formal postvention support process in Gateshead for someone who has been bereaved by a drug or alcohol related death, but there are informal processes.
During Drug and Alcohol related death review meetings, for example, other individuals who may be at risk or affected by the death are identified, and the appropriate service reaches out to offer advice or support to help reduce further harm or deaths.
Specialist drug and alcohol treatment and recovery services in Gateshead can also offer support directly to family who contact the service following a death. If people accessing the service are affected by a death, the service will reach out and offer support and further harm reduction advice, such as trauma therapy and counselling.
While there is more structured support available within Gateshead from bereavement or mental health organisations in the area, it is not widely known about and may leave bereaved communities feeling unsure of where to turn to for support.
Embracing a compassionate place approach would support those experiencing loss unexpectedly from suicide, as the impact of grief and loss would be better understood by society and those impacted offered support by their wider communities, including the workplace.
Preventing harm and future deaths from alcohol, drugs and suicide

Good jobs, safe homes, strong communities and access to health and social support are the foundations of a healthy life. When these building blocks are missing or broken, people are more vulnerable to death and harm from alcohol, drugs and suicide. Efforts to prevent harm are often focused on specific individual interventions (30), like the system and services factors; however, addressing these issues requires co-ordinated action across multiple factors and sectors beyond healthcare.
Solutions addressing the social, political, economic, and commercial factors that impact health have the greatest potential impact, as they affect the whole population (30) and do not require high levels of individual agency or behaviour change. These approaches aim to reduce harm at the population level, before people reach crisis or become ill.
Gateshead's Health and Wellbeing Strategy provides an action framework across society, as a joined up, whole system approach; we call this the Population Intervention Triangle. The triangle focuses on three areas:
- Civic-level interventions: tackling social, political and economic factors like licensing laws and housing policies.
- Service-based interventions: offering high-quality care and support for those affected
- Community-centred interventions: engaging with people's lived experiences to co-design solutions
To reduce harm, Gateshead can act across these levels, strengthening the seams where these approaches meet, to create a cohesive, whole-system response.

While harm from alcohol, drugs and suicide can affect anyone, some groups are at much higher risk. Effective prevention requires targeted approaches tailored to specific risk factors, alongside universal strategies that address the entire population. The prevention pyramid is informed by a wide range of existing research, theory, and frameworks on prevention, and helps frame these efforts (205-212). Universal approaches target the entire population, such as campaigns to raise awareness about alcohol harm or mental health support. Targeted interventions focus on high-risk groups, such as young people, those in poverty, or individuals with mental health issues. Crisis responses and harm reduction provide immediate help for people already struggling, from suicide prevention to addiction treatment. Postvention supports those left behind after a death, aiming to prevent further harm.

By applying this model within Gateshead's civic, service and community efforts, we can take wide-ranging, co-ordinated actions to save lives.



Hopes for the future
This report has tackled difficult topics, revealing how deeply lives in Gateshead are affected by losses to alcohol, drugs and suicide. Each loss leaves an absence that is profoundly felt. These heartbreaking stories remind us of the urgency to act and inspire a collective resolve for change.
Across Gateshead, inspiring work is already underway. Community support groups and innovative prevention programmes are bringing people together with a shared commitment to ensuring no one faces these challenges alone:
We have groups with like-minded people that share experience, strength, and hope. And by doing that, we're giving back to newcomers who are coming in the rooms for the first time, realising that they're not alone. That is a massive thing. We're not alone. It really, really, really helps.
This determination to connect and support others highlights the power of community:
The ways we can help to change experiences for other people is don't be afraid to talk to somebody, anybody. We can have open conversations with each other.
The efforts taking place in Gateshead give us every reason to hope, as communities create empowering, safe and inclusive spaces. These efforts are not just transforming lives - they're saving them. Yet, we still have work to do. To make a lasting difference, we must continue to challenge stigma, invest in prevention, and ensure help is available to everyone who needs it, when they need it. Lived experience is at the heart of this change, as we celebrate the courage and resilience of those who share their stories:
I'm still here. That's the best I can say some days. But I'm here because someone showed me I wasn't invisible. That's all it took - a moment of care to remind me I mattered.
Gateshead's strength lies in its people, in their compassion, their determination and their willingness to shape a future defined by hope and recovery. Together, we can ensure Gateshead is a place where everyone thrives.
If you are struggling, please know:
You are not alone.
You are seen.
And there is always hope.
Key recommendations
At the beginning of this report, I wrote about the importance of hearing from people who have experienced the far reaching and indiscriminate effects of harm caused by alcohol, drugs and suicide which ripple far and wide.
This report highlights that whilst these issues can affect anyone, sadly it is the people in our most disadvantaged communities that are the worst affected.
We have seen how inequalities faced by people in our community, starting from conception and throughout life, often lead to poor health and lives being cut short from alcohol, drugs and suicide.
But we are determined to reduce inequalities, giving everyone the best start in life, empowering and maximising capabilities, and providing the support needed throughout to thrive, so everyone can lead healthy and fulfilling lives.
We must act together across multiple sectors to achieve this.
1 - Co-production with people with lived experience
'Nothing about us without us'
Supporting the Thrive pledge of 'putting people and families at the heart of everything we do', and the Health & Wellbeing Strategy commitment to 'make sure that all local people can contribute to and engage with the future of Gateshead', we want to increase the voices of lived experience in the development, co-production and evaluation of our strategies and service delivery plans, including children, young people and adults.
This includes meaningful approaches across our partnerships to involving people with lived experience, where their knowledge and expertise is valued.
We envisage organisations who build capacity and capability for this work, drawing on the principles of equity, diversity and inclusion by working with a range of individuals with lived experience.
Recognising the role of our VCSE organisations in Gateshead in supporting people and reaching into communities, we will work collaboratively as set out in our Gateshead Compact Agreement 2024-27.
2 - Challenging Stigma
'Stigma kills'
We all have a responsibility to reduce stigma surrounding mental health, alcohol and drug use, self-harm, and suicide.
I envisage our communities and organisations across Gateshead, understanding that problems caused by alcohol, drugs and suicide are not a personal choice, resulting in people receiving the same quality support as those dealing with other health issues.
Starting with the language we use, organisations should have a clear communications strategy that ensures the right language is used, as recognised and supported by people with lived experience. Reducing the negative impacts of stigmatising language.
The focus of our strategies, policies, plans, communication and training, needs to shift from a narrow lens of personal responsibility to one where we recognise and address the factors and inequalities that can lead to these circumstances.
The learning and development needs of our workforce should be considered in challenging stigma, extending the reach of initiatives such as Recovery Ally Training which helps increase understanding of the language of recovery and to provide support without judgement.
We must create conditions that maximise the chances for our people to recover from addiction according to their own needs and strengths. We can do this by making Gateshead a recovery place, which promotes visible recovery and challenges stigma. We achieve this by embracing the principles of inclusion, recovery and integration, using a whole-system approach. This involves partnership working with community organisations, specialist treatment services, policymakers, people in recovery, employers, and neighbours.
3 - Give every child the best start in life
'An ambition for all children'
To improve and protect health for future generations, giving our children the best start in life is the most important thing we can do.
Gateshead seeks to create supportive and healthy environments where all children can thrive, breaking the cycle of adversity and promoting wellbeing.
Reducing the impacts of childhood adversity requires community and civic-level action to strengthen resilience and reduce health inequalities that can lead to ill health, and harm from alcohol, drugs and suicide.
We want to see a whole-systems approach to supporting our children and young people's health and wellbeing, where resources and decision making is prioritised towards their needs. To do this we need to learn from the findings of our recent Children and Young Peoples mental health needs assessment, mobilising as system to take forward the recommendations.
This includes promoting an alcohol-free childhood; identifying young carers for parents with alcohol, drugs and mental health concerns and providing much-needed support; nurturing, inclusive and safe school environments; and strengthening support for care experienced children and young people across the system.
We must continue to tackle poverty at every opportunity, ensuring that the resources are available for the support services, to lessen the damaging effects of poverty. This means offering different things in different places, reaching for equity.
4 - Making health equity everyone's goal
'Why treat people and send them back to the conditions that made them sick?'
We must continue to prioritise the eight Marmot Principles as set out in our Health and Wellbeing Strategy, to tackle the inequalities happening in our communities, leading to ill health and harm from alcohol, drugs and suicide.
But we can't do this alone, it is everyone's responsibility.
'Health in all Policies' (HiAP) provides a framework to help address complex issues linked to alcohol, drugs and mental health, across sectors. Making it a reality, means making health equity a goal for everyone. It is vital, that health and wellbeing is considered in its broadest sense, with a strong acknowledgement of the building blocks of health, and parity given to outcomes related to alcohol and drug use, mental health, self-harm, and suicide.
This needs to be reflected in the design, delivery, and evaluation of strategies and plans, such as the developing Gateshead Suicide Prevention Plan, Gateshead Drug and Alcohol Strategy, Children and Young People's strategy, and many others across the system that address the building blocks of health, such as the Local Plan and Economic Development Strategy.
Employers in Gateshead have a vital role to play in influencing the conditions in which people work and live and, consequently, their health. Promoting health and wellbeing goes beyond awareness campaigns and can be achieved through good quality jobs and working conditions that provide parity for mental wellbeing, support financial wellbeing and reduce the impact of stigma through training and effective anti-bullying policies.
Unemployment can be a significant time of stress, this needs to be recognised and understood as a system, with psychological support offered to reduce the risk of harm caused by alcohol, drugs and poor mental health and wellbeing.
5 - A place-based approach to tackling health inequalities
'Working effectively as a system, putting people and families at the heart of what we do'
Equitable, accessible services are vital for those who are experiencing the harms from alcohol, drugs, self-harm, and suicide. To do this we must understand the needs of communities experiencing increased risk of harm, with inequalities identified and built in to planning and evaluation of services. This includes continued use of trauma informed approaches to reduce barriers and create safe, sensitive and trusted services.
To better understand the health inequalities faced by our most vulnerable communities, we must improve the data and knowledge we collect and share with partners. This includes understanding the needs of the groups experiencing inequalities as highlighted in this report, and increased understanding of self-harm, online harms across all-ages, and the impact of domestic abuse.
It is important that our response to this issue is not solely focused on the services we provide when people are already experiencing harm, and it is vital we address the factors that lead to harm in the first place.
To do this, we need to consider action for Gateshead through the Population Intervention Triangle, as set out in the Health and Wellbeing Strategy. This ensures we strengthen the building blocks of health on a societal and community level.
There is a need to increase protective factors for people and communities, drawing on the strengths of local assets, to prevent deaths from alcohol, drugs and suicide. This means understanding what our communities need and what they have to offer.
6 - Tackling the commercial determinants of health
'Putting people before profit'
In last year's report, I brought attention to the tactics used by the smoking, alcohol, gambling and fast-food industries and the harm and devastation caused by these unhealthy commodities.
Action must be taken to reduce harm from health-damaging industries including alcohol, gambling and social media.
This includes supporting and advocating the Balance Blueprint for Reducing Alcohol Harm, using our local systems such as advertising and licensing policies to protect children and vulnerable adults, and continuing to challenge the narrative of the alcohol industry that focuses on personal responsibility and poor choices.
We must continue to recognise the harm caused by gambling as a public health issue, advocating for a comprehensive public health approach to gambling harm prevention, and building our knowledge and capability of this issue locally, to support communities in Gateshead.
Online harms and the impact of social media are increasingly part of our world. When considering the environments we live in and how they impact health, we must not forget the digital platforms we navigate. As we develop our response to suicide prevention, we must consider the impact of online harms and work together with communities to advocate for safer online environments, including the role of media corporations in responsibly reporting deaths from alcohol, drugs or suicide.
7 - Making Gateshead a Compassionate Place
'Transforming life and death though the healing powers of compassion and community'
The harm from alcohol, drugs, and suicide ripples across people and communities. Any loss can be difficult to bear, and bereavement due to alcohol, drugs and suicide can evoke difficult feelings and lead to isolation. Those experiencing terminal illness due to alcohol and drugs, may face further inequalities at the end of life.
I believe that Gateshead is well placed to embrace a Compassionate City approach and create the conditions to improve end of life and bereavement care for all, including vital and timely bereavement support and bereavement-friendly workplaces for the people in our community who experience the devastating ripple effects of these deaths.
We need a shared vision of Compassionate Gateshead, where we can build on the numerous assets that already exist, from commissioned services, charities, and compassionate individuals who are dedicated to improving the lives of people working, living and dying in Gateshead.
Acknowledgements
This report was made possible thanks to the courage and bravery of the people who shared their stories and experiences. They did this in the hope of helping and making a difference for others, for which we are incredibly grateful. To those who participated - thank you. We see you; we hear you, and we stand with you.
Enabling people with lived experience to be involved in this report, required the help, support, knowledge, and kindness of people and organisations working in Gateshead. Thank you to those who helped do this, and who also guided this report on its use of sensitive, inclusive and supportive language:
Deacon Tracey Hume, Recovery Church
Ricky Vasey and Emma Ferguson, Recovery Connections
Shannon Scott and Marie Bewley, If U Care Share
Sara Muzaffar, Peace of Mind
Talking about dying and death literacy was enabled through the work and contribution of Dr Lizzie Woods, Consultant in Palliative Medicine, Gateshead NHS Health Foundation Trust. Thank you, Lizzie, for your help navigating this topic.
A huge thank you to the team who worked incredibly hard putting this report together:
- Sophie Colebourne
- Allison Cowling
- Rebecca Dew
- Angela Hannant
- Claire McNaney
- Olivia Mullaney
- Yvonne Robson
- Barbara Rowan
- Julia Sharp
- Phil Snow
- Louise Sweeney
The recorded lived experience stories shared in this report were developed by the talented team at Digital Voice for Communities.
This report was supported by the Gateshead Health Determinants Research Collaboration, supporting and enabling research in practice.
References
(3) Camacho C, Webb RT, Bower P, Munford L. Risk factors for deaths of despair in England: An ecological study of local authority mortality data. Social Science & Medicine. 2024 Feb 1;342:116560.
(4) Institute for Health Metrics and Evaluation. GBD Compare. (opens new window)
(7) Walsh D, McCartney G, Minton J, Parkinson J, Shipton D, Whyte B. Deaths from 'diseases of despair' in Britain: comparing suicide, alcohol-related and drug-related mortality for birth cohorts in Scotland, England and Wales, and selected cities. J Epidemiol Community Health. 2021 Dec;75(12):1195-201.
(8) Zero Suicide Alliance. Substance Misuse (opens new window)
(9) Alcohol Profile | Fingertips | Department of Health and Social Care (opens new window)
(10) Area Profile; Alcohol, Fingertips | Department of Health and Social Care (opens new window)
(12) Opiate and crack cocaine use: prevalence estimates - GOV.UK (opens new window)
(15) Suicides in England and Wales by local authority - Office for National Statistics (opens new window)
(16) Transport D for. Road Safety Data (opens new window)
(19) Alcohol-specific deaths in the UK - Office for National Statistics (opens new window)
(20) Alcohol-specific deaths in the UK - Office for National Statistics (opens new window)
(22) Suicide Prevention - Data | Fingertips | Department of Health and Social Care (opens new window)
(23) Fingertips | Department of Health and Social Care (opens new window)
(24) Gateshead Council: Population estimates and projections
(25) NDTMS - ViewIt - Adult (opens new window)
(28) GOV.UK. Suicide prevention strategy: action plan (opens new window)
(29) Gilmore AB, Fabbri A, Baum F, Bertscher A, Bondy K, Chang HJ, et al. Defining and conceptualising the commercial determinants of health. The Lancet. 2023 Apr 8;401(10383):1194-213.
(30) Pirkis J, Dandona R, Silverman M, Khan M, Hawton K. Preventing suicide: a public health approach to a global problem. The Lancet Public Health. 2024 Oct 1;9(10):e787-95.
(31) Addressing the leading risk factors for ill health - The Health Foundation (opens new window)
(32) Jones L, Sumnall H. Understanding the relationship between poverty and alcohol misuse.
(33) WHO. Closing the gap in a generation. 2008 (opens new window)
(35) Samaritans. Online Excellence Programme (opens new window)
(36) Samaritans. How social media users experience self-harm and suicide content (opens new window)
(37) Kalinin VV, Hocaoglu C, Mohamed S. Anxiety Disorders: The New Achievements. BoD - Books on Demand; 2021. 210 p.
(38) NCISH. Annual report 2023: UK patient and general population data 2010-2020 (opens new window)
(39) Molly Russell: Coroner's report urges social media changes. BBC News (opens new window)
(41) Samaritans. Samaritans' media guidelines for reporting suicide (opens new window)
(42) Domaradzki J. The Werther Effect, the Papageno Effect or No Effect? A Literature Review. International Journal of Environmental Research and Public Health. 2021 Jan;18(5):2396.
(43) Petticrew M, Maani N, Pettigrew L, Rutter H, Van Schalkwyk MC. Dark Nudges and Sludge in Big Alcohol: Behavioral Economics, Cognitive Biases, and Alcohol Industry Corporate Social Responsibility. The Milbank Quarterly. 2020;98(4):1290-328.
(44) Thomas S, Cowlishaw S, Francis J, van Schalkwyk MCI, Daube M, Pitt H, et al. Global public health action is needed to counter the commercial gambling industry. Health Promotion International. 2023 Oct 1;38(5):daad110.
(45) GOV.UK. Gambling-related harms evidence review: summary (opens new window)
(46) Samaritans. Gambling-related harms and suicide (opens new window)
(47) Royal College of Psychiatrists, Alcohol Concern. A Losing Bet? Alcohol and gambling: investigating parallels and shared solutions. 2013 Feb.
(49) Dowling NA, Cowlishaw S, Jackson AC, Merkouris SS, Francis KL, Christensen DR. Prevalence of psychiatric co-morbidity in treatment-seeking problem gamblers: A systematic review and meta-analysis. Aust N Z J Psychiatry. 2015 Jun;49(6):519-39.
(50) Yarbakhsh E, van der Sterren A, Bowles D. Screening and Treatment for Co-occurring Gambling and Substance Use: A Scoping Review. J Gambl Stud. 2023 Dec 1;39(4):1699-721.
(51) Gong Y, Palmer S, Gallacher J, Marsden T, Fone D. A systematic review of the relationship between objective measurements of the urban environment and psychological distress. Environment International. 2016 Nov 1;96:48-57.
(52) Congdon P. Geographical Patterns in Drug-Related Mortality and Suicide: Investigating Commonalities in English Small Areas. International Journal of Environmental Research and Public Health. 2019 Jan;16(10):1831.
(53) Kim K, Lee DW, Jung SJ. Role of individual deprivation and community-level deprivation on suicidal behaviors: Insights from the UK Biobank study. SSM Popul Health. 2024 Mar 20;26:101654.
(54) Suicides in England and Wales - Office for National Statistics (opens new window)
(55) Suicides in England and Wales by local authority - Office for National Statistics (opens new window)
(57) Alcohol-specific deaths in the UK - Office for National Statistics (opens new window)
(60) YoungMinds. Understanding trauma and adversity | Resources (opens new window)
(66) Barnes, A., Snell, C., Bailey, A., Loopstra, R., Cheetham, M., Morris, S., Power, M., Davies, H., Scott, M., Taylor-Robinson, D., Pickett, K. APPG Child of the North - Child Poverty and the Cost of Living Crisis. A report prepared for the APPG Child of the North. 2022.
(67) Barnardo's. Neglected Minds: A report on mental health support for young people leaving care. 2017 Sep.
(68) Alderson H, Brown R, Copello A, Kaner E, Tober G, Lingam R, et al. The key therapeutic factors needed to deliver behavioural change interventions to decrease risky substance use (drug and alcohol) for looked after children and care leavers: a qualitative exploration with young people, carers and front line workers. BMC Medical Research Methodology. 2019 Feb 21;19(1):38.
(69) The Care Leavers Association. 2016. What is a Care Leaver. (opens new window)
(74) Evans R, White J, Turley R, Slater T, Morgan H, Strange H, et al. Comparison of suicidal ideation, suicide attempt and suicide in children and young people in care and non-care populations: Systematic review and meta-analysis of prevalence. Children and Youth Services Review. 2017 Nov 1;82:122-9.
(77) Health Matters: Preventing drug misuse deaths - UK Health Security Agency. 2017 (opens new window)
(82) McManus S, Bebbington P, Jenkis R, Brugha T. Mental Health and Wellbeing in England. Adult Psychiatric Morbidity Survey 2014. Leeds: NHS Digital;
(84) Shirzad M, Yenokyan G, Marcell AV, Kaufman MR. Deaths of despair-associated mortality rates globally: a 2000-2019 sex-specific disparities analysis. Public Health. 2024;35-42.
(85) YoungMinds. Understanding trauma and adversity | Resources (opens new window)Personal well-being in the UK - Office for National Statistics [Internet]. [cited 2024 Nov 25]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/bulletins/measuringnationalwellbeing/october2016toseptember2017
(86) Michniewicz KS, Bosson JK, Lenes JG, Chen JI. Gender-atypical mental illness as male gender threat. American Journal of Men's Health. 2016;10(4):306-17.
(87) NHS England » LGBT+ health (opens new window)
(88) Samaritans. LGBTQ+ communities and suicide (opens new window)
(89) Institude of Alcohol Studies. LGBTQ+ People and Alcohol. 2021 Jul.
(90) Murray S, Holloway K, Buhociu M. "It's called homophobia baby" exploring LGBTQ + substance use and treatment experiences in the UK. Drugs: Education, Prevention and Policy. 2024 Sep 2;31(5):505-15.
(91) GOV.UK. Drug misuse: Findings from the 2013/14 Crime Survey for England and Wales (opens new window)
(93) Public Health Wales. Neurodiversity. (opens new window)
(94) NHS England | Workforce, training and education. 2023. Neurodiversity (opens new window)
(95) Autistic people and suicidality (opens new window)
(96) GOV.UK. Suicide prevention in England: 5-year cross-sector strategy (opens new window)
(97) Banaschewski T, Coghill D, Zuddas A. Oxford Textbook of Attention Deficit Hyperactivity Disorder. Oxford University Press; 2018. 473 p.
(98) Young S, Sedgwick O. Attention deficit hyperactivity disorder and substance misuse: an evaluation of causal hypotheses and treatment considerations. Expert Review of Neurotherapeutics. 2015 Sep 2;15(9):1005-14.
(99) Young S, Woodhouse E. Assessment and treatment of substance use in adults with ADHD: a psychological approach. J Neural Transm. 2021 Jul 1;128(7):1099-108.
(100) Johnson J, Morris S, George S. Managing Comorbid Attention Deficit Hyperactivity Disorder (ADHD) in Adults With Substance Use Disorder (SUD): What the Addiction Specialist Needs to Know. Addictive Disorders & Their Treatment. 2021 Sep;20(3):181.
(101) Fuller-Thomson E, Rivière RN, Carrique L, Agbeyaka S. The Dark Side of ADHD: Factors Associated With Suicide Attempts Among Those With ADHD in a National Representative Canadian Sample. Archives of Suicide Research. 2022 Jul 3;26(3):1122-40.
(102) Giupponi G, Giordano G, Maniscalco I, Erbuto D, Berardelli I, Conca A, et al. Suicide risk in attention-deficit/hyperactivity disorder. Psychiatr Danub. 2018 Mar;30(1):2-10.
(103) Balazs J, Kereszteny A. Attention-deficit/hyperactivity disorder and suicide: A systematic review. World Journal of Psychiatry. 2017 Mar 22;7(1):44.
(106) NHS England » Perinatal mental health (opens new window)
(108) MBRRACE-UK. Saving Lives, Improving Mothers' Care. 2023 Oct.
(109) Wyse JJ, Lovejoy J, Holloway J, Morasco BJ, Dobscha SK, Hagedorn H, et al. Patients' perceptions of the pathways linking chronic pain with problematic substance use. Pain. 2021;162(3):787-93.
(111) Tang NKY, Crane C. Suicidality in chronic pain: a review of the prevalence, risk factors and psychological links. Psychological Medicine. 2006;36(5):575-86.
(112) Too LS, Spittal MJ, Bugeja L, Reifels L, Butterworth P, Pirkis J. The association between mental disorders and suicide: A systematic review and meta-analysis of record linkage studies. Journal of Affective Disorders. 2019 Dec 1;259:302-13.
(113) Public Health England. Better care for people with co-occurring mental health and alcohol/drug use conditions. 2017 Jun.
(114) National Institute for Health and Social Care. Severe mental illness and substance misuse (dual diagnosis): community health and social care services. 2016 Sep.
(115) Definition | Background information | Self-harm | CKS | NICE (opens new window)
(117) Alcohol Profile - Data | Fingertips | Department of Health and Social Care (opens new window)
(118) GOV.UK, 2018. The public health burden of alcohol: evidence review (opens new window)
(119) Bloomfield K. Understanding the alcohol-harm paradox: what next? The Lancet Public Health. 2020 Jun 1;5(6):e300-1.
(120) Fingertips | Department of Health and Social Care (opens new window)
(121) PDF: Health and Wellbeing (opens new window)
(122) In-work poverty trends - The Health Foundation (opens new window)
(123) Leng G. The Impact of Homelessness on Health, A Guide For Local Authorities. LGA. 2017;
(124) Samaritans. To thrive, not just survive. 2023.
(125) Nolte-Troha C, Roser P, Henkel D, Scherbaum N, Koller G, Franke AG. Unemployment and Substance Use: An Updated Review of Studies from North America and Europe. Healthcare (Basel). 2023 Apr 20;11(8):1182.
(126) Nagelhout GE, Hummel K, de Goeij MCM, de Vries H, Kaner E, Lemmens P. How economic recessions and unemployment affect illegal drug use: A systematic realist literature review. International Journal of Drug Policy. 2017 Jun 1;44:69-83.
(127) GOV.UK Review of drugs part two: prevention, treatment, and recovery (opens new window)
(128) Mental health at work (opens new window)
(131) Keyes KM, Hatzenbuehler ML, Hasin DS. Stressful life experiences, alcohol consumption, and alcohol use disorders: the epidemiologic evidence for four main types of stressors. Psychopharmacology. 2011 Mar 5;218(1):1.
(132) Walling MA. Suicide Contagion. Curr Trauma Rep. 2021 Dec 1;7(4):103-14.
(133) World Health Organisation. Mental health and forced displacement (opens new window)
(135) Murphy D, Ashwick R, Palmer E, Busuttil W. Describing the profile of a population of UK veterans seeking support for mental health difficulties. Journal of Mental Health. 2019 Nov 2;28(6):654-61.
(136) Murphy D, Turgoose D. Exploring patterns of alcohol misuse in treatment-seeking UK veterans: A cross-sectional study. Addictive Behaviors. 2019 May 1;92:14-9.
(137) Gateshead JSNA: Ex-armed forces personnel and their dependents.
(138) Rodway C, Ibrahim S, Westhead J, Bojanić L, Turnbull P, Appleby L, et al. Suicide after leaving the UK Armed Forces 1996-2018: A cohort study. PLoS Med. 2023 Aug;20(8):e1004273.
(139) Gateshead Council. Gateshead Domestic Abuse Needs Assessment. 2024.
(142) Domestic Homicide Project - VKPP Work (opens new window)
(143) Dobash RE, Dobash RP. Contacts with the Police and Other Agencies across the Life-Course of Men Who Murder an Intimate Woman Partner. Policing: A Journal of Policy and Practice. 2016;10(4):408-15.
(144) Vatnar SKB, Friestad C, Bjorkly S. The Influence of Substance Use on Intimate Partner Homicide: Evidence from a Norwegian National 22-year Cohort. International Journal of Forensic Mental Health. 2019;18(2):99-110.
(146) Bridger E, Strang H, Parkinson J, Sherman LW. Intimate Partner Homicide in England and Wales 2011-2013: Pathways to Prediction from Multi-agency Domestic Homicide Reviews. Cambridge Journal of Evidence-Based Policing. 2017;93-104.
(147) Fingertips | Department of Health and Social Care (opens new window)
(148) Hertzberg D, Boobis S. The Unhealthy State of Homelessness 2022: Findings from the Homeless Health Needs Audit. Homeless Link; 2022 Oct.
(149) Health matters: rough sleeping - GOV.UK (opens new window)
(150) Office for National Statistics [Internet]. 2023 [cited 2024 Sep 25]. Drug-related deaths and suicide in offenders in the community, England and Wales: 2011 to 2021. Available from: Drug-related deaths and suicide in offenders in the community, England and Wales: 2011 to 2021
(152) Identification and brief advice could reduce alcohol harm, survey says | The BMJ (opens new window)
(153) GOV.UK Widening the availability of naloxone (opens new window)
(155) GOV.UK Alcohol and drug prevention, treatment and recovery: why invest? (opens new window)
(156) Stigma Kills | NHS Addictions Provider Alliance (opens new window)
(157) Luna A. The Components of Dehumanization. Peace and Conflict Studies. 2015 May 1;22(1):18-33.
(160) NHS Inform: Challenging drug and alcohol stigma (opens new window)
(161) Batchelder AW, Glynn TR, Moskowitz JT, Neilands TB, Dilworth S, Rodriguez SL, et al. The shame spiral of addiction: Negative self-conscious emotion and substance use. PLOS ONE. 2022 Mar 18;17(3):e0265480.
(162) Alcohol Change UK. Challenging the stigma around alcohol (opens new window)
(164) McKenzie SK, Oliffe JL, Black A, Collings S. Men's Experiences of Mental Illness Stigma Across the Lifespan: A Scoping Review. Am J Mens Health. 2022 Jan 1;16(1):15579883221074789.
(165) Chatmon BN. Males and Mental Health Stigma. Am J Mens Health. 2020 Jul 1;14(4):1557988320949322.
(166) Lamb R, Kougiali ZG. Women and shame: narratives of recovery from alcohol dependence. Psychology & Health. 0(0):1-38.
(167) Majumder P. Exploring stigma and its effect on access to mental health services in unaccompanied refugee children. BJPysch Bulletin. 2019;275-81.
(168) Jennifer S McCleary, Patricia J Shannon, Tonya L Cook. Connecting Refugees to Substance Use Treatment: A Qualitative Study. Social Work in Public Health. 2016;31(1):1-8.
(170) Sveen CA, Walby FA. Suicide Survivors' Mental Health and Grief Reactions: A Systematic Review of Controlled Studies. Suicide and Life-Threatening Behavior. 2008 Feb;38(1):13-29.
(171) Feigelman W, Gorman BernardS, Jordan JohnR. Stigmatization and Suicide Bereavement. Death Studies. 2009 Aug;33(7):591-608.
(172) Exploring stigma and its effect on access to mental health services in unaccompanied refugee children - PubMed (opens new window)Cleveland Clinic [Internet]. [cited 2024 Oct 15]. What is grief? Available from: https://my.clevelandclinic.org/health/diseases/24787-grief
(173) Scocco P, Preti A, Totaro S, Corrigan P, Castriotta C. Stigma, grief and depressive symptoms in help-seeking people bereaved through suicide. Journal of Affective Disorders. 2019 Feb 1;244:223-30.
(175) Jordan JR, McIntosh JL. Grief After Suicide: Understanding the Consequences and Caring for the Survivors. Routledge; 2011. 575 p.
(176) Cerel J, Maple M, van de Venne J, Moore M, Flaherty C, Brown M. Exposure to Suicide in the Community: Prevalence and Correlates in One U.S. State. Public Health Rep. 2016;131(1):100-7.
(177) Miklin S, Mueller AS, Abrutyn S, Ordonez K. What does it mean to be exposed to suicide?: Suicide exposure, suicide risk, and the importance of meaning-making. Social Science & Medicine. 2019 Jul 1;233:21-7.
(178) Pitman A, Osborn D, King M, Erlangsen A. Effects of suicide bereavement on mental health and suicide risk. The Lancet Psychiatry. 2014 Jun 1;1(1):86-94.
(179) Abrutyn S, Mueller AS. Are Suicidal Behaviors Contagious in Adolescence? Using Longitudinal Data to Examine Suicide Suggestion. Am Sociol Rev. 2014 Apr 1;79(2):211-27.
(180) Young IT, Iglewicz A, Glorioso D, Lanouette N, Seay K, Ilapakurti M, et al. Suicide bereavement and complicated grief. Dialogues in Clinical Neuroscience. 2012 Jun;14(2):177.
(181) Lander L, Howsare J, Byrne M. The Impact of Substance Use Disorders on Families and Children: From Theory to Practice. Social work in public health. 2013;28(0):194.
(182) Eng J, Drabwell L, Stevenson F, King M, Osborn D, Pitman A. Use of Alcohol and Unprescribed Drugs after Suicide Bereavement: Qualitative Study. International Journal of Environmental Research and Public Health. 2019 Oct 24;16(21):4093.
(183) Cain AC. Survivors of suicide. Springfield, Ill. : Thomas; 1972 (opens new window)
(184) Cerel J, Brown MM, Maple M, Singleton M, Van De Venne J, Moore M, et al. How Many People Are Exposed to Suicide? Not Six. Suicide & Life Threat Behav. 2019 Apr;49(2):529-34.
(185) Cerel J, McIntosh JL, Neimeyer RA, Maple M, Marshall D. The Continuum of "Survivorship": Definitional Issues in the Aftermath of Suicide. Suicide and Life-Threatening Behavior. 2014;44(6):591-600.
(186) Pirkis J, Bantjes J, Gould M, Niederkrotenthaler T, Robinson J, Sinyor M, et al. Public health measures related to the transmissibility of suicide. The Lancet Public Health. 2024 Oct 1;9(10):e807-15.
(187) Identifying and responding to suicide clusters.
(188) Waegemakers Schiff J, Lane AM. PTSD Symptoms, Vicarious Traumatization, and Burnout in Front Line Workers in the Homeless Sector. Community Ment Health J. 2019 Apr 1;55(3):454-62.
(189) Suicide prevention and postvention | NHS Employers (opens new window)
(190) About Blue Light Together (opens new window)
(192) GOV.UK Government response to the independent review of drugs by Dame Carol Black (opens new window)
(193) GOV.UK Review of drugs: summary (accessible version) (opens new window)
(194) Samaritans. The economic cost of suicide in the UK (opens new window)
(195) Webb L, Yarwood G, Witham G, Wright S, Galvani S. Providing holistic end-of-life care for people with a history of problem substance use: a mixed methods cohort study of interdisciplinary service provision and integrated care. BMC Palliative Care. 2024 Apr 1;23(1):86.
(196) Quesada J, Hart LK, Bourgois P. Structural Vulnerability and Health: Latino Migrant Laborers in the United States. Medical Anthropology. 2011 Jul 1;30(4):339-62.
(198) Hudson BF, Flemming K, Shulman C, Candy B. Challenges to access and provision of palliative care for people who are homeless: a systematic review of qualitative research. BMC Palliative Care. 2016 Dec 3;15(1):96.
(199) Stajduhar KI, Mollison A, Giesbrecht M, McNeil R, Pauly B, Reimer-Kirkham S, et al. "Just too busy living in the moment and surviving": barriers to accessing health care for structurally vulnerable populations at end-of-life. BMC Palliative Care. 2019 Jan 26;18(1):11.
(200) Abel J. Compassionate communities and end-of-life care. Clin Med (Lond). 2018 Feb;18(1):6-8.
(201) Kellehear A. Compassionate Communities Civic Charter (opens new window)
(202) Scocco P, Idotta C, Totaro S, Preti A. Addressing psychological distress in people bereaved through suicide: From care to cure. Psychiatry Research. 2021 Jun 1;300:113869.
(203) Pitman AL, Rantell K, Moran P, Sireling L, Marston L, King M, et al. Support received after bereavement by suicide and other sudden deaths: a cross-sectional UK study of 3432 young bereaved adults. BMJ Open. 2017 May 1;7(5):e014487.
(204) Jordan JR, McIntosh JL, Bolton IM, Campbell FR, Harpel JL, Linn-Gust M. A Call to Action: Building Clinical and Programmatic Support for Suicide Survivors. In: Grief After Suicide. Routledge; 2010.
(205) Butler JC. 2017 ASTHO President's Challenge: Public Health Approaches to Preventing Substance Misuse and Addiction. Journal of Public Health Management and Practice. 2017 Sep;23(5):531-6.
(206) Martineau F, Tyner E, Lorenc T, Petticrew M, Lock K. Population-level interventions to reduce alcohol-related harm: An overview of systematic reviews. Preventive Medicine. 2013 Oct 1;57(4):278-96.
(207) Begun DA. Ch. 2: Prevention and the Continuum of Care (opens new window)
(208) Prevention | Local Government Association (opens new window)
(211) Danese A, Asmussen K, MacLeod J, Meehan A, Sears J, Slopen N, et al. Revisiting the use of adverse childhood experience screening in healthcare settings. Nat Rev Psychol. 2024 Nov;3(11):729-40.
(212) Hawk KF, Vaca FE, D'Onofrio G. Reducing Fatal Opioid Overdose: Prevention, Treatment and Harm Reduction Strategies. Yale J Biol Med. 2015 Sep 3;88(3):235-45.
A note about the data and terms used in this report
Data on suicide
In England and Wales, when somebody dies unexpectedly, a Coroner investigates the circumstances to establish the cause of death. The investigation, referred to as an 'inquest,' is a process that can take months, and in some cases, years. When an inquest has concluded, the death is officially registered.
The figures for suicide include deaths that are registered within the calendar year, rather than deaths occurring in the calendar year due to the long registration process. 39% of deaths registered in 2023 had a date of death in the same year, 51% occurred in 2022 and the remaining deaths occurred in 2021 or earlier.
Data on suicide includes all deaths from intentional self-harm (for those aged 10 years and above). It also includes deaths caused by injury or poisoning of undetermined intent (for those aged 15 years and above), based on the assumption that the majority of these deaths will be suicide. This is referred to as the National Statistics definition of suicide.
The area data on suicide is based on the persons usual residence, so does not take into account people that have travelled to end their life. Calculating rates, allows us to make comparisons between geographic areas over time. The rates show the age-standardised mortality rate (ASMR) of deaths per 100,000 people.
Data on deaths related to drug poisoning (23)
The data from ONS on deaths from drug misuse are a directly standardised rate of deaths per 100,000 and based on a 3-year rolling period. The data comes from a wider data set - Deaths related to drug poisoning. Those deaths directly attributed to drug misuse are included within this subset.
As with suicide, the figures show the deaths registered rather than deaths occurring in each calendar year. Due to the length of time, it can take to complete a coroner's inquest, it can take months or even years for a drug related death to be registered. Therefore, it is impossible to compare the numbers in the ONS data to the numbers we review in our local Drug Related Death process which we undertake when notified of a suspected drug related death.
Public Health England, and previously the National Treatment Agency for Substance Misuse recommended that a confidential inquiry should be undertaken following a drug related death. In Gateshead this process is referred to as a drug related death (DRD) review and all suspected DRDs are discussed within the review process. Drug-related deaths need to be reviewed in a timely manner to identify learning, or actions, which may reduce the risk of further deaths attributed to drugs. This may happen before a coroner's inquest has taken place, to review specific cases, where we suspect the death may be as a direct consequence of drugs, (drug related death), and take learning from these cases that could implement change to reduce drug related deaths. This process involves numerous statutory and non-statutory agencies to ascertain common themes and learning.
Caution regarding data for the reporting of deaths related to alcohol, drugs and suicide
Drug-related death figures reported by the Office for National Statistics (ONS) are categorised as either 'drug poisoning' or 'drug misuse.'
'Drug poisoning' deaths involve a broad spectrum of substances, including controlled and non-controlled drugs, prescription medicines and over-the-counter medications. They also include accidents, assaults and suicides involving drug poisonings, as well as deaths from drug abuse and drug dependence.
'Drug misuse' deaths are defined as a drug poisoning with one or both of the following conditions:
- The underlying cause is drug abuse or drug dependence
- Involvement of any controlled substance under the Misuse of Drugs Act 1971 (201)
The inclusion of suicides within drug poisoning deaths can result in "double-counting" where one death is included in the figures for suicide, as well as a drug-related death (213).
By focusing this report on data looking at deaths by drug misuse rather than drug poisoning, we have aimed to reduce the potential magnitude of double counting, although it cannot be excluded. If unintentional double counting has occurred, it is likely to be small numbers.
Deaths from alcohol, drugs and suicide do not exist in isolation, for example some drug poisoning deaths involve alcohol and it is often not possible to establish the primary substance responsible for the death (201)(213). In some cases a death recorded as an alcohol or drug-related death were a suicide, however in the absence of evidence such as a suicide note, it will be recorded as an alcohol or drug-related death.
Change to the standard of proof for suicide in England and Wales
In 2018 in England and Wales there was a change to the standard of proof - the level of evidence needed by coroners when determining whether a death was caused by suicide. This was lowered from the criminal standard of 'beyond reasonable doubt' to the civil standard of 'on the balance of probabilities' (202).
A report by the ONS concludes that this change did not significantly impact suicide rates, noting that the factors behind increasing suicide rates are likely to be complex (214).
