Chapter 3: The direct impact of COVID-19 in Gateshead
Covid-19 in numbers in Gateshead
The statistics help to show the big picture, but we mustn't forget that behind every number lies a human story.
13,772 Covid-19 cases (12 March 2020 to 30 April 2021)
499 deaths where Covid-19 was mentioned on the death certificate (23 March 2020 to 30 April 2021)
1433 Covid-19 hospitalisations at Queen Elizabeth Hospital in Gateshead (23 March 2020 to 30 April 2021)
Between March 2020 and the end of April 2021, we experienced two Covid-19 epidemic 'waves'. The first wave started in March 2020 and ended at the end of May 2020. The second wave started at the beginning of September 2020 and ended at the end of April 2021 (ONS, 2021).
(ONS (2021) Coronavirus (COVID-19) Infection Survey technical article: waves and lags of COVID-19 in England, June 2021 (opens new window))
Confirmed Covid-19 cases (Gov.uk (2021)
(GOV.UK Coronavirus data, people vaccinated (opens new window)) (ONS (2021) Population Estimates for UK, England and Wales, Scotland and Northern Ireland: mid-2020-april-2021- geography (opens new window))
| Gateshead | North East | England | |
| Wave 1 12 March 2020 to 31 May 2020. There was limited community testing during wave 1 in the community so actual case numbers in Wave 1 are underrepresented. | 1 in 163 people with Covid-19 | 1 in 189 people with Covid-19 | 1 in 260 people with Covid-19 |
| Wave 2 1 September 2020 to 30 April 2021 | 1 in 16 people with Covid-19 | 1 in 15 people with Covid-19 | 1 in 16 people with Covid-19 |
In the first wave, the rate of confirmed Covid-19 cases was higher in Gateshead than in the North East as a whole, and England.
In the second wave, the rate of confirmed cases was in parallel with England, but slightly lower than the North East as a whole.
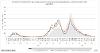
The first wave peaked at a seven day rolling rate of 122 cases per 100,000 residents of Gateshead on 10th April 2020. The second wave peak, on 4th January 2021, was over three times higher than this at 479 cases per 100,000. However, this was lower than England and the North East (Gov.Uk, 2021) 10 (ONS, 2021). (ONS (2021) Population Estimates for UK, England and Wales, Scotland and Northern Ireland: mid-2020-april-2021- geography, ONS filter outputs 2021 (opens new window))
Hospitalisations
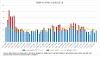
| Number of patients treated | percentage of all diagnosed cases in Gateshead | |
| Wave 1 | Approximately 500 | Approximately 40% |
| Wave 2 | Approximately 900 | Approximately 7% |
Due to the time lag of cases arriving at hospital, Wave 1 at the QE hospital took place between 23 March 2020 to 31 August 2020 and Wave 2 occurred from 1 September 2020 to 30 April 2021 Hospitalisation data provided by Gateshead Health NHS Foundation Trust.
Deaths
During Wave 1, there were 237 deaths where Covid-19 was mentioned on the death certificate (18% of all diagnosed cases). In Wave 2, the number was 262 deaths where Covid-19 was mentioned on the death certificate (2% of all diagnosed cases). In Wave 2, more deaths took place in hospitals and less in care homes. (ONS (2021) Death registrations and occurrences by local authority and health board.)

Excess deaths were also experienced in two waves. In Wave 1, the number of excess deaths far exceeded the average for the five years, 2015-2019, with a high proportion of these excess deaths attributable to Covid-19.13 Excess deaths in Wave 2 were much lower, as was the proportion attributable to Covid-19. A high number of deaths is sometimes followed by a period of below-average deaths, due to vulnerable people and those with pre-existing conditions dying sooner than expected. Although there is some evidence of this, this displacement does not account for the excess mortality seen at the beginning of the pandemic, suggesting Covid-19 affected more people than just those who were expected to die in the following days, weeks and months. (4 ONS (2021) Excess mortality and mortality displacement in England and Wales: 2020 to mid-2021. ONS Covid-19 effect on death occurrences (opens new window))
Disproportionate impact of Covid
Age
The first wave was characterised by a slightly older age profile with almost 50% of cases in those aged 60+. In Wave 2, approximately 75% of cases were evenly spread over the working age population (Gov.Uk, 2021). (Gov.uk (2021) Coronavirus (COVID-19) in the UK GOV.UK Coronavirus data, people vaccinated (opens new window))
This may reflect the limited community testing available at the beginning of the pandemic. The age profile of Queen Elizabeth Hospital inpatients differed over the course of the year, with the first wave characterised by an older inpatient profile (79% of cases aged 65 and over). The second wave had a slightly younger profile with just 65% of cases aged 65 and over.
Ethnicity
Mortality from Covid-19 was also higher in some ethnic groups. Evidence from the ONS, ONS deaths due to Covid (opens new window), suggests during the period 24 January 2020 - 31st March 2021, after only adjusting for age, people from all ethnic groups, with the exception of Chinese and White Other, had at least a 25% increased risk of death when compared to people from White British backgrounds.
People from a Bangladeshi background were around four times as likely to die from Covid-19 than White British ethnicities. After adjusting for age, measures of disadvantage, occupation, living arrangements and pre-existing health conditions, men from Bangladeshi and Black African ethnicities were still almost twice as likely to die from Covid-19 than men from White British ethnicities.

Deprivation
The majority of Gateshead residents (approx. 60%) live in the 30% most deprived Middle Layer Super Output Areas (MSOAs - a small geographic area of between 2000-6000 households). Covid-19 deaths data from the ONS mapped to MSOA level reveals that over the course of March 2020 to April 2021, 62% of deaths were in these communities.
Although there were local nuances to the way different communities were affected at different stages of the pandemic, typically poorer outcomes were seen in the most deprived areas (ONS, 2021). (ONS (2021) Deaths due to COVID-19 - Interactive map.ONS deaths due to Covid - interactive map (opens new window))
Illness and loss
A few years ago, my mam had a major kidney transplant. My dad had to donate a kidney to save my mam's life, which was magnificent. Not just life changing, but lifesaving.
In September, after my first day at work, I felt a little bit breathless and my muscles were aching, despite having had the vaccine in August. The whole household came down with Covid and it was terrifying!
My mam spent a week in hospital with no visitors and bad breakfasts (running joke), relying on video calls to speak to her each day. We were all worried.
Us left in the house. Me, my dad and brother were waiting for news constantly. How is she? What's happening? The doctors were keeping us posted and after a long week, she was home!
We have recovered since. I'm in the apprenticeship I've always wanted. My dad's working from home and my mam is almost back to work. Normality once more (almost).
Alfie Gascoigne
I developed Covid in April 2020. I woke with a sore throat and because of my placement thought it best to get tested which initially came back as negative.
The following day, I began to develop different symptoms, sometimes only lasting a couple of hours at a time, such as nausea, diarrhoea, change in temperature and I also had a persistent headache which weren't the typical symptoms.
I was very tired but, as I lived on my own, I could just lay about and sleep most of the day which was helpful - although on the second and third evening I went to bed and it was a bit concerning as I developed a pain in my upper back and my breathing pattern changed.
I had my phone with me by my pillow in case this became unmanageable and I would need to call for help but thankfully this wasn't needed.
The following week as the symptoms subsided and I could go out again, I walked to post a letter which was about 500 yards from my home and called 111 on my return as I couldn't get my breath and was told this was normal and would gradually ease.
I returned to work after 10 days and just had enough energy to get through a shift and would be exhausted when I returned home, I would become breathless quite easily. The tiredness gradually eased, and I started to exercise again to improve my breathing.
In April 2021, I started having what I now know to be asthma attacks. I have recently had tests which have indicated very strong levels of inflammation in my airways and now taking regular medications to help get this under control with a confirmed asthma diagnosis.
Dawn Harvey, Gateshead Council
"You don't miss people until they are gone." Service user, Age UK Gateshead "I lost my husband to Covid, I then lost my sister. I have never felt so angry, helpless, lost but most of all scared. I'm alone. I'm not old. I feel cheated, I cry every day, sometimes all day."
Service user, Age UK Gateshead
As someone who organises and officiates at funerals and church services, I have witnessed first-hand some of the isolation and distress caused by the pandemic.
When a loved one dies, we say farewell in a way that best honours the one we have lost and gives most comfort to those who grieve. The pandemic prevented this from happening. Very few were allowed to attend funerals. Social distancing had to be observed so that, quite often, families could not sit together. Face coverings had to be worn. Hymn singing was not allowed. Services had to be kept as brief as possible. All of this added to the distress already being suffered by the bereaved.
Following a funeral, we normally benefit from the companionship of family and friends and the pandemic again impacted hugely on this. The bereaved, particularly those who live alone, were forced into a painful isolation, unable to have visitors or to go out and about themselves. The effect of this cannot be overstated.
Telephone calls and video calls have been immensely important in helping to ease slightly the dreadful loneliness.
Adele Phillips, Minister/Celebrant
Health and social care services face massive challenges
Covid-19 presented challenges of unprecedented proportions to health and social care services. Services had to transform overnight, with staff asked to take on different roles, and facing intense levels of pressure and uncertainty, whilst trying to maintain non-Covid related essential services. In the early stages, there was a shortage of personal protective equipment (PPE).
Writing as a GP who has worked in Gateshead for 34 years, in practice at Rowlands Gill until 2014 and latterly in Urgent and Unscheduled Care, which includes in and out of hours care, I have been part of our local primary care response to the Covid pandemic. This was a new disease with an uncertain means of transmission and a wide range of presentations.
It made some people a bit unwell but made others very ill, very quickly. Across the country many people were dying. Everybody, patients and staff alike, was frightened.
'Hot Hubs'
Because of the risk of infection with Covid, Gateshead's GP practices could not provide safe care at their surgeries and so, as a response to the need to see, assess and treat patients who could have Covid, dedicated 'hubs' were established, one at Blaydon GP Surgery based in the Blaydon Leisure Centre and another at Second Street Surgery in central Gateshead.
Establishing these two hubs required the coordinated efforts of staff from CBC Health (Gateshead's Urgent and Unscheduled Care provider), Gateshead's GP community, Gateshead's Community Nursing Teams and Gateshead Council staff.
Patients were referred to appointments at these two centres where GPs from across the borough volunteered to provide the care needed, supported by nursing and administrative staff who also volunteered to support these hubs.
'Hot Home Visiting'
Provision of care to patients, who were unable to travel to the 'hot hubs', was also arranged with the development of a 'hot' home visiting service. The home visiting service was based at Bensham Hospital with GPs working alongside the staff of the community nursing Rapid Response Team. Patients requiring assessment at home would be referred to the 'hot' service and seen by a member of the GP team.
North East Ambulance Service provided the vehicles and the drivers necessary to support the visiting clinicians and these drivers were integral in ensuring the safety of the clinicians.
New skills and patterns of working were developed. 'Donning' (putting on PPE) and 'doffing' (taking off PPE) at the back of a car, sometimes in the sunshine but also when it was windy or raining, took a degree of teamwork to ensure that infection risk was minimised. Running water to wash hands after patient contacts came from a water bottle. Gateshead's response from primary care has been an example of coordinated and supportive teamworking.
Alexander Liddle, GP, CBC Health Gateshead
At the beginning of the pandemic, staff working in primary care were as shocked as anyone and trying to process what was happening.
Some patients were scared to come into the practice, some staff were worried about coming to work as at that point we didn't fully know or understand the risks and people were terrified.
We had to review and rewrite all of our infection control policies to protect staff and patients in the practices and plan new ways of working.
NHS England recommended the use of remote consultations to maintain safe service delivery and protect our patients and staff so overnight we had to implement and adapt to a new way of working, which was tough as our GPs like to see patients face to face, but suddenly we had to use remote consultation methods like telephone and video. Some of the patients really like this now though.
At the beginning of the pandemic when we were setting up the 'hot' site, we struggled to get PPE. On one occasion we were sent out of date masks. Staff didn't feel that paper masks were adequate, so we had to buy our own PPE. We had lovely support from the community who rallied round to help. A local garage provided disposable seat covers for GPs going into people's home, a group made scrubs for us and bags to wash them in. They shouldn't have needed to, and we should have been able to access the PPE we needed.
Teresa Graham, Business Partner and Practice Manager, Second Street Surgery, Oxford Terrace and Rawling Road Medical Group & CBC Health GP Federation.
During the pandemic, there has been immense pressure trying to deliver to a high level of service to our patients to the best of our capability.
When GPs had to stop most face-to face appointments, at the beginning of the pandemic, we had more people coming to us for community pharmacist advice - some of those needed referrals back to GPs. We were seeing more people but only allowed two people in the shop at a time and we had to deal with all of the day-to-day running and also various changes occurring with Covid protocols.
Our working hours changed from 45 hours a week to about 70 hours a week. Even after the shop closed, we were still providing home prescription deliveries. Our prescription home delivery service increased by about 100%.
We always advised people with Covid-19 symptoms not to come into the pharmacy, but some still did. That was scary. Some community pharmacists, as with other frontline NHS staff, caught Covid from their interactions with patients and many have lost their lives trying to help others.
Community Pharmacist
At the Queen Elizabeth Hospital in Gateshead, we have a state of the art laboratory with cutting edge diagnostic and screening technology. Our team of highly trained, dedicated biomedical scientists and support staff provide a 24-hours a day seven days a week testing service. During the Covid-19 pandemic, our laboratory team has used their expertise to set up a Covid-19 testing laboratory that can process thousands of samples a week.
Our laboratory is part of a dynamic network of NHS laboratories that works across the North East and Cumbria to ensure all patients in our region have access to the testing they need.
As a member of the infection team, I have been involved with all aspects of managing Covid-19 in the hospital. Patients who have been to the hospital during the pandemic will have noticed many changes. There are dedicated areas for assessing and treating patients with Covid-19. We have been involved in the latest research trials; bringing in specialist treatments as they are available. We have set up a staff and patient Covid-19 testing service which has allowed us to keep areas of the hospital Covid-19 free and protect the vital services we provide to our patients.
The safety of our patients in the hospital and community is of the highest importance to us. Our infection prevention and control team have worked collaboratively with our community partners and all clinical teams in the hospital to make sure our patients are protected from Covid-19 whilst they are receiving care with us.
At the Gateshead Health NHS Foundation Trust, we have dedicated, expert, caring staff who work with and for the people of Gateshead. Covid-19 has presented us with many challenges, I am proud to be part of a team that has worked so hard throughout the pandemic to look after our patients.
Dr Alice Wort, Consultant Microbiologist, Gateshead Health NHS Foundation Trust.
One of the scariest things is that I don't know where I caught Covid - but I know it was during a fortnight's annual leave from work. I was terrified when I was taken to hospital - but even in my moments of horror, people went above and beyond to make me feel comfortable.
My paramedic, James, put on the music I like, Nirvana and Red-Hot Chili Peppers, to make me more comfortable. And through A&E I was treated like a VIP, I'll never forget it. My experience was utterly flawless. Ward 1 staff were amazing. I went there during the night, but every single member of staff introduced themselves to me, which has massive value. I felt like an individual, not just a patient, and that people genuinely cared for me. They were so professional and fastidious with their hygiene and PPE. Even the food was smashing - the catering was always fabulous, and I looked forward to mealtimes!
Thank you from the bottom of my heart - you all have my sincere gratitude.
Cheryl Gascoigne, patient, Gateshead Health NHS Foundation Trust
Pre-Covid we would look after people who had extensive surgery. They came in critically ill from various diseases and we had a routine, we would be able to come in, assess the situation and carry out the care of those patients who were critically ill, very ill indeed, but we would manage that and hopefully see most of those recover.
During the pandemic, we're seeing patients come into the department who have been extremely ill, and we're used to seeing patients who are extremely ill, but these are on a different level. We found we were having to cope with patients who would have to be positioned prone (carefully putting a patient into the prone position flat on their front and face down, rather than on their back, to try and help them breathe more easily) often, regularly. We would have deaths in terrible circumstances, relatives weren't allowed to be there and we, as the nursing staff for Covid and non-Covid patients, had to deal with the demise of a patient ourselves. I often put a phone to a person's ear when they were passing away, so that their close relatives could say their goodbyes.
So I'd leave shift on a number of occasions - well most of the time - upset, stressed and exhausted. My resilience now has diminished massively. I would be able to leave my work at work, be able to put it outside my car door to go home. But now I can't. I bring things home with me and have to click into a different mode and I struggle to do that. But I think as things start to ease, I'm hoping to do that.
Aurial Reay, Critical Care Sister, Gateshead
When the pandemic occurred, we worked closely with public health colleagues and the Infection, Prevention and Control (IPC) Team at the Queen Elizabeth Hospital, as part of our community services response. These well-established relationships ensured an integrated, seamless and consistent approach to care home, domiciliary care, promoting independence centres, community and acute hospital services and primary care in terms of infection prevention and control across Gateshead.
We implemented a number of changes with the IPC Team, including:
- extending their access to seven days a week for advice and support
- undertaking planned site visits to any care home or facility or provider that needed it across Gateshead
- carrying out environmental assessments to manage outbreaks or giving advice on prevention
- leading and delivering 'donning' and 'doffing' training (putting on and taking off personal protective equipment (PPE)) for all staff in both acute, community, care homes, and private providers and lay carers if required
- working collectively with community nursing teams to provide targeted interventional prevention into care homes that were either in outbreak or had come out of outbreak and needed to maintain Covid free sites
- supporting the national mandate to train every staff member in care homes across Gateshead in IPC, handwashing, PPE and management of Covid and in total trained over 2400 staff in just over two weeks
- working with community services and the Council's Public Health Team to deliver the swabbing (lateral flow) directive for patients and staff, again training, supporting and advising. This was on top of supporting the acute hospital with their Covid response and their other elements of work including pressure damage management and support, and other IPC advice still necessary but not related to Covid-19.
Nicola Allen, Chief Executive, CBC Health Ltd.
Focus on care homes
Care homes have been hit particularly hard by the pandemic, especially in the early months.
At the beginning of the pandemic, there was an awful lot of Covid in the community. The company and staff who didn't have it worked so hard to keep the home going.
To support the NHS, we set up a unit for people who had Covid-19 and were being discharged from hospital and couldn't go home as they either didn't have a care package in place or were from a different care home that couldn't take patients with Covid-19. These were new residents who didn't know our staff - this was the hardest thing for me and my team.
At the beginning of the pandemic, before the unit for residents with Covid opened, we had difficulty in getting PPE. Our normal supplier couldn't provide it and the company drove round all over trying to get it. Also, it took time to get training on donning and doffing PPE. It felt as though care homes were left out. I think it's been a real lesson from the pandemic that social care is there to support the NHS.
These were really difficult times for staff. We had a cry every Thursday - I don't know what it was about a Thursday, but we used to have a breakdown and cry.
The social distancing was very hard for residents. At the beginning we kept everyone two metres apart even in the lounges, and only two people to a table in the dining room. Staff wore masks which made it difficult for communication with residents. After two months you could really see the impact that this was having on residents. So, we did a risk assessment and put residents together in bubbles of two who could sit next to each other in communal areas.
To keep people in contact with their families, we had window visits, tablets for Zoom meetings and encouraged telephone calls. We put in an extra telephone line. Staff were the bridge between their families and a loved one. Some residents' families, their husbands or wives are elderly, and we've supported them as much as residents over the last two years.
Care Home Manager, Gateshead
Staff make an awful situation a whole lot better by testing us, giving us PPE and letting us sit downstairs or in garden with dad. But even I notice how staff and my dad seem weary and need some relatives' intervention.
My dad came straight from hospital last year, I've never seen the lounge where he spends his days and so look forward to a cuppa and a game of bingo with the people he spends his life with now.
Care home resident's daughter
Mam went into a care home on a respite basis in March 2020. The home had a lovely atmosphere and I used visit regularly, without having to make an appointment, taking my granddaughter with me. Mam had her birthday that month. There were many members of the family there to help her celebrate.
The next day, the care home went into lockdown due to Covid. It was terrible, we could no longer visit mam and we felt she would think she had been abandoned by her family. When we called her on the phone it just wasn't the same due to mam's dementia and the fact that she couldn't see us.
Today mam is a shell of her former self. Visits have to be made by appointment only and the time we actually have with mam is approximately 30 minutes. Only five members of the family are allowed on the visiting list. Mam has a beautiful baby great granddaughter she has yet to meet, and I only hope she will get to meet her one day.
Care home resident's daughter
Next - Chapter 4: Coming together to respond to the pandemic
